When she was diagnosed with a rare form of gynaecological cancer in 2015, Zowie Fussey from Ulceby, North Lincolnshire, could barely have imagined where she’d be ten years later on.

Zowie Fussey during her cancer treatment
The former administrative worker and then mum-of-two to Keaton and Martin was diagnosed with a granulosa cell tumour, a rare form of ovarian cancer, at the age of just 33. Zowie needed a radical hysterectomy and nine weeks of intensive chemotherapy at the Queen’s Centre, Castle Hill Hospital, in order to treat the disease.
But the ‘all clear’ wasn’t the only thing that Zowie was left with when she was finally discharged from the hospital’s care. Zowie had been so moved by the kindness and compassion shown to her while she was a patient of the Cottingham-based oncology unit that she now had a desire to give something back.
Driven by the care she’d received and her consultants’ determination to give her the best chance at life, she now wanted to pay that forward and promptly made a pact with herself: manage two years in remission, and train to become a nurse.
“I’m a firm believer in everything happens for a reason,” says Zowie.
“The staff at the Queen’s Centre were just brilliant. I knew from the start that my consultants, Mr Theo Giannopoulous and Dr George Bozas, were really rooting for me, they were going to do everything they could to get me through, and the Clinical Nurse Specialists were so supportive and reassuring throughout.

Zowie shares a bottle of bubbly with her cousin Jenna
“I received my treatment on Ward 30 and through the chemotherapy day unit, and all of the staff there; nurses, doctors, care assistants, volunteers, domestics; were just so kind. I expected a cancer centre to be a bit of a sad place, if I’m honest, but the staff were just so jolly and really helped to keep myself and my family positive.
“They allowed my family to attend appointments with me; my husband, my mum and my cousin Jenna; and this was so important to me, that not only could my family know what was happening, but that they were involved in my care journey too.
“No way did I expect to be sitting there laughing and joking while I was having my chemotherapy treatment, but that was all thanks to the environment the staff created for their patients, one of hope and positivity.
“The staff really made my cancer journey an experience which would shape my outlook on life and my future career, it was a gift in some ways, and one which I’m now hoping to use to give back to other patients and families with cancer.”
In 2017, Zowie landed a job working as a healthcare assistant at St Hugh’s Hospital in Grimsby, a role which gave her an ‘in’ into the world of healthcare and which she credits as having taught her the basics of good patient care.
But by 2019, Zowie had done some soul-searching and, staying true to her word, more than two years cancer-free, she began to research courses at the University of Hull so she could train to become a nurse.
“I wanted to be a nurse to help other people in the way that I’d been supported as a patient. While I worked placements in different hospital departments, I really knew that I wanted to become a research nurse and to give people the time, and the hope, that I ‘d been given.

Zowie says her family were a huge support
“Many years ago, I worked in an admin role in a research team, and during my cancer treatment, I would often be wheeled past the clinical trials office in the Queen’s Centre and be curious about what they did in there. The more I thought about it, the more I knew that this was the area I wanted to work in.”
Zowie started her nurse training in September 2019, studying all through the Covid pandemic, and qualified in the summer of 2022 thanks to a combination of campus-based study, remote learning, hospital placements and a dissertation on oncology research.
Having studied beauty therapy while in between jobs, she went back to volunteer at a number of Look Good, Feel Better sessions, held at the Queen’s Centre, which offer help to manage the physical effects of cancer treatment; a service she had benefited from herself as a hospital patient.

Zowie is loving her new role as a cancer research nurse
Zowie continued to top up her clinical experience at local NHS hospitals and St Hugh’s while studying for her nursing degree, then joined St Hugh’s as a staff nurse once she qualified. Then when the opportunity came up to join the academic oncology and haematology research team at Castle Hill, Zowie jumped at the chance.
“I didn’t get the job first time,” she says. “I was really disappointed, but at the same time, it made me more determined than ever to secure a place in the team. I asked Tania, the senior research nurse manager of the academic oncology and haematology trials unit, what else I could do or what extra training I needed to stand a better chance next time, then I went off and did it. So when another job came up towards the end of last year, I really hoped it was my time to shine.”
Now aged 43, and 10-years cancer-free, Zowie is eight weeks into her new role as a clinical research nurse working within the Queen’s Centre’s academic oncology and haematology research team. Her role will involve supporting eligible patients into research trials for new cancer treatments, including medications or vaccines, with a view to prolonging and/or improving patients’ quality of life.
“My new team has been so friendly and welcoming, it feels like I’ve been here forever,” Zowie says.
“I’ve bumped into a few people already who I recognise from my days as a patient, who looked after me on the ward, and often they remember me too; one nurse, Emma, even remembered the ‘thank you’ bracelet I gave her. It’s amazing to think that, of all the patients these people must see, week in week out, that you can still have an impact on them in the same way they impact on you.
“It’s a real privilege to be in this role now. I know I’m a small cog in a big wheel but we’re all working to improve outcomes for our patients. Some areas of nursing can be incredibly pressurised, but the research role will allow me the time to get to know my patients, to provide that extra care and compassion, and that means everything to me.”
 Dr Debbie Wearmouth, Infection Doctor at Hull University Teaching Hospitals, said: “We are asking visitors to wear masks in wards, clinics and clinical departments to help us protect our patients, already vulnerable through illness and injury, so they don’t catch these potentially serious illnesses.
Dr Debbie Wearmouth, Infection Doctor at Hull University Teaching Hospitals, said: “We are asking visitors to wear masks in wards, clinics and clinical departments to help us protect our patients, already vulnerable through illness and injury, so they don’t catch these potentially serious illnesses. Dr Wearmouth is also urging people who are already ill or showing signs of flu, diarrhoea and vomiting or other respiratory illnesses not to come to hospital to visit patients.
Dr Wearmouth is also urging people who are already ill or showing signs of flu, diarrhoea and vomiting or other respiratory illnesses not to come to hospital to visit patients.














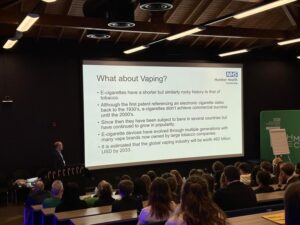 Some teachers volunteered to carry out spirometry tests, used to measure lung function, to highlight the importance of good lung health.
Some teachers volunteered to carry out spirometry tests, used to measure lung function, to highlight the importance of good lung health.


