Parents are being warned of potential new health dangers posed by vaping and cannabis use among children and young people.
A case study published by doctors from Hull in the Cureus Journal of Medical Science discusses the case of a 15-year-old rushed to Hull’s A&E with chest pain and difficulty breathing.
The young person, who admitted to using cannabis and to vaping an average of 500 puffs every day, was also experiencing swelling to the neck and face, low oxygen levels and a high heart rate.
A CT scan allowed medics to diagnose ‘air leak syndrome’, in which pockets of gas or air had collected in parts of the body including the spinal canal, between the lungs, and under the skin.
Air leak syndrome is, as yet, not formally recognised as one of the conditions which constitutes e-cigarette or vaping associated lung injury (EVALI), but doctors believe the young person’s use of cannabis and vapes is a likely cause* of internal damage to their food and/or wind pipe, and in turn this led to pockets of air collecting outside of their lungs.
And while some of the tiny air pockets may naturally have resolved themselves over time, for some patients air leak syndrome can go on to cause life threatening health issues.
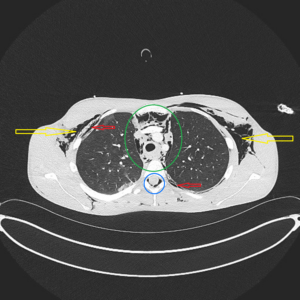
Above: A CT scan identified pockets of air around the spinal canal
Dr Ragda Abdallah, one of the study’s co-authors, says: “Vaping and the use of e-cigarettes is illegal in the UK for under 18s, yet their popularity is still rising rapidly, with recent research** suggesting that one in every five UK children aged 11 to 17 has now tried vapes.
“In the case of our study subject, this young person had been vaping quite intensely for around a year at the same time as inhaling cannabis. As a team of researchers, we know that one patient’s experience is not enough to draw any firm conclusions, but it does lead us to question whether air leaks are a further, potentially under-recognised complication of vaping and cannabis inhalation in young people.
“At this time, there have been only a few other similar reported cases, predominantly involving adults, reported worldwide.”
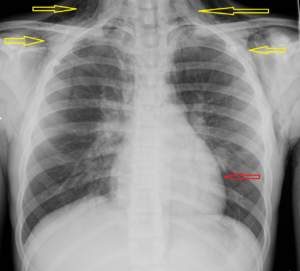
Above: An X-ray helps to diagnose air leak syndrome
Dr Abdallah continues: “For any parent, seeing your child rushed to A&E with chest pain, their face swollen, pulse racing and struggling to breathe, must be absolutely terrifying.
“Thankfully, staff were able to diagnose air leak syndrome and begin the appropriate treatment very quickly, but this still involved a 10-day stay in the paediatric high dependency unit (PHDU) where the young person was nil-by-mouth for a week and required intensive oxygen therapy through a mask.
“While much more research into long-term effects is needed, this case study sends a clear warning about the rare but potential side-effects of using vapes in particular.
“It’s also an indicator that we, as medical professionals, should be more open to the idea of damage caused by vaping or cannabis inhalation when looking for potential causes of chest pain and breathing difficulties in adolescents.”
Scott Crosby, Associate Director for the Centre for Excellence; a regional prevention programme tackling the three biggest killers; tobacco, alcohol and unhealthy food and drink, said:
“Protecting children from vaping harms is essential. Strong regulation is needed to reduce youth appeal and tackle illegal, unsafe devices, which often bypass safety standards and are linked to organised criminal supply chains.
“As the Chief Medical Officer says: ‘If you smoke, vaping is much safer; if you don’t smoke, don’t vape.’ Legal, regulated vapes help adult smokers quit, but no young person should ever use them. We support the Tobacco and Vapes Bill, which will tighten controls, strengthen penalties, and improve licensing to shut down the illicit market and protect children.”
Notes to Editor
Potential Association of Air Leak Syndromes With E-cigarette or Vaping Product Use-Associated Lung Injury (EVALI) was published in the Cureus Journal of Medical Science on 28 September 2025, authored by Dr Chidi Anakebe, Dr Ragda Abdallah, Dr Mahil Abdalla, Dr Fatima Taha, and Dr Haji Sheeraz Khan.
* Subsequent testing identified infections (flu and streptococcus pathogens) which may also have contributed to the patient’s acute illness.
** Use of vapes among young people in Great Britain, published by ASH, July 2025.
According to the UK Government, smoking and vaping are understood to cause around 80,000 preventable deaths in the UK every year.
















 Michaela said: “It’s important that patients living with dementia and their families get the right care and support when they’re admitted to hospital – and once they’re back home.
Michaela said: “It’s important that patients living with dementia and their families get the right care and support when they’re admitted to hospital – and once they’re back home.