- Reference Number: HEY-324/2016
- Departments: Gynaecology
- Last Updated: 1 June 2016
Introduction
This leaflet has been produced to give you general information about your surgery. Most of your questions should be answered by this leaflet. It is not meant to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
What is urinary stress incontinence?
Urinary stress incontinence occurs when a woman leaks urine when they exercise, cough, sneeze or laugh. It usually happens because the muscles and tissues that make up the pelvic floor have become weak or damaged. The pelvic floor works like a sling that goes from the pubic bone in the front, to the base of the spine at the back. It supports the urethra which is the tube which carries urine down from the bladder. When the pelvic floor is strong and can keep the urethra in the right position, the urethra can form a tight seal so that urine does not leak out. If the pelvic floor is damaged or weak, it does not support the urethra properly. So when a person moves and there is pressure on the urethra, it moves out of position. The tight seal is lost and urine leaks out.
What is a transobturator tape (TOT) procedure?
This is the procedure for urinary stress incontinence and it is performed under a general or spinal anaesthetic.
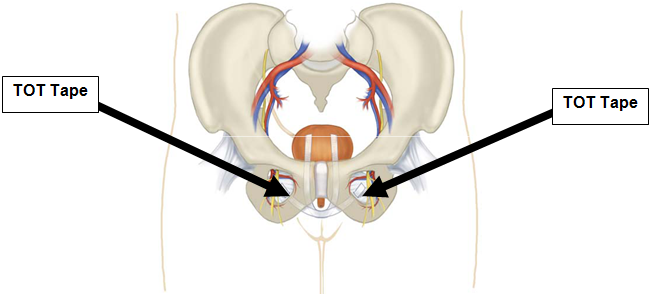
A small incision is made on the wall of the vagina and the permanent tape is introduced via the vagina to sit under the urethra. The needles used to place the tape are introduced through small incisions at both sides of your upper inner thigh (see picture). The tape used is a permanent mesh, which will not be dissolved in your body.
Surgery for stress incontinence aims to give you more control over your bladder. It cannot always cure the problem completely.
Why do I need a transobturator tape (TOT)?
You will have discussed the options to manage your stress incontinence with your doctor and decided to have a transobturator tape inserted.
What are the risks or complications?
Serious complications are rare with this type of surgery. However, no surgery is without risk and the potential complications are:
- Bladder irritability (urgency symptoms or overactive bladder) after surgery (5 – 10%).
- Risk of damage to the vagina, bladder, urethra or blood vessels which will require further surgery (2 – 3%).
- Risk of urinary tract infections (1 – 5%).
- Difficulty passing urine, which will require self-catheterisation after the surgery usually for a few weeks (1 – 5%).
- Risk of a wound infection (1%).
- Risk of mesh becoming infected or rejected which would require the tape to be removed (1%).
- Risk of blood clots in the legs or chest (1%).
- This procedure is not aimed at improving any urgency symptoms, which are likely to persist and may deteriorate.
- Small risk of tape eroding into nearby organs e.g. vagina or urethra.
- Small risk of pain in groin or thigh, associated with the tape.
- Risk of bleeding.
What is the success rate?
Success rates after the procedure is between 82 – 96% [National Institute of Clinical Excellence (NICE) – Patient Information 2005].
Surgical procedures for stress urinary incontinence are not usually suitable if you still plan to have children, or think you might want to in the future.
How do I prepare for my transobturator tape (TOT)?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
Pre-admission clinic appointment
You will be asked to attend the pre-admission clinic. At this appointment the nurse will have explained the operation and have gone through your admission and discharge details with you. If you need any help at home with dependent relatives or would like to speak to a social worker, please speak to the staff at the pre-admission clinic or the ward for more information. Blood tests, heart tracing and an X-ray will have been done, as necessary, ready for your operation.
What will happen on the day of my procedure?
You will normally be admitted to the ward the day before your surgery or on the morning of your surgery. We will also be able to answer any questions you might have and prepare you for your operation.
Before going to theatre you will be seen by the anaesthetist who will go through the anaesthetic procedure with you. If you are having a period this will not stop us from performing your operation.
You will be given advice about when to stop eating and drinking.
You will be asked to have a bath or a shower on the morning of your operation. If you have been at home, please have a shower before your admission. Do not use talcum powder or body sprays. Remove all makeup, nail varnish and jewellery. Weddings rings can be worn (they can be covered with tape).
Before going to theatre you will be asked to put on the hospital gown. You will also be asked to put on white knee length or thigh length compression stockings. The compressions stockings will help to reduce the risks of blood clots in your legs. The compression stockings must be worn until you are fully mobile. You may also be given a small injection of a blood-thinning agent. This will continue daily until you are fully mobile or go home. When you go to theatre, a nurse will walk with you to theatre.
Will I be sleepy before going to theatre?
Often no pre-medication is given, but if you feel particularly anxious the anaesthetist will prescribe a tablet to help you relax. (If you do have a pre-med you will be taken down to theatre in your bed).
What will happen afterwards?
After your operation you will go to the recovery room until you are well enough to return to the ward. The nurses looking after you will check your blood pressure, pulse and look for any bleeding from your wounds and vagina.
You may have a drip in your arm; this will give you all the fluid you need until you are drinking normally again. When you get back to the ward you will be allowed sips of water; we will increase the amount you can drink slowly as this will help to prevent you from being sick.
You may have some pain and discomfort after your surgery. To keep you comfortable, we will give you regular pain relief medication.
You may have a catheter in the bladder (to drain the urine) and you may have a vaginal pack (dressing) in your vagina for up to 24 hours after the surgery. If other surgery (e.g. vaginal repair) has been performed at the same time, the catheter may be kept in for a few more days and you will be in hospital for 3 – 4 days.
If you do not have a catheter, you will be encouraged to pass urine and an ultrasound scan may be performed to check that you are able to empty your bladder.
How long will I be in hospital?
You may be in hospital for an overnight stay depending on how your bladder function is after the surgery.
What can I expect during my recovery?
Your recovery should be fairly quick and you will be able to return to light activities after 1 – 2 weeks. You may pass small stitches or have light vaginal bleeding/discharge. You will be given pain relief medication after the surgery to take when required. If you develop symptoms of urinary tract infection (burning or stinging as you pass urine) or have a persistent offensive vaginal discharge, you should see your GP.
What should I avoid after my surgery?
You should avoid the following:
- Sexual intercourse or using tampons for 4 – 6 weeks to help any wound to heal.
- Constipation (see dietetic advice below to avoid constipation).
- Heavy lifting (more than 15kgs) to avoid recurrence of your problem.
- Excessive weight gain to avoid recurrence.
- Smoking because it can increase the risk of failure.
If you want advice on how to stop or reduce smoking please contact the Hull and East Riding Stop Smoking service (free phone 0800 0915 5959).
What should I do after surgery?
You should drink plenty of fluids (6 to 8 glasses per day) and eat a balanced diet with plenty of fresh fruit and vegetables to help keep your bowels regular. Eating plenty of foods rich in fibre will also help (e.g. porridge, bran, cereal, brown bread).
You should make sure you do not drink too much tea or coffee as this may irritate the bladder (maximum 3 cups per day). Make sure you drink 1.5 to 2 litres of fluid per day.
When will I be able to drive?
You will be able to drive 2 – 4 weeks after surgery. Provided you are comfortable sitting in a car seat and can perform an emergency stop without pain or discomfort, it is safe to drive. We strongly advise you to check with your insurance company first, as many companies have strict guidelines and time frames with regards to driving after surgery.
What if I have problems after discharge?
If you have problems you should contact your GP in the first instance. Nursing staff on the ward are always happy to answer any queries that you may have.
Will I have a follow up appointment at the hospital?
You will be seen in the outpatient clinic 6 – 8 weeks after your surgery.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact:
Gynaecology Outpatients, Women and Children’s Hospital – (01482) 607829.
Ward 30, Women and Children’s Hospital – (01482) 382739 / 604387.
Useful information
Royal College of Obstetricians and Gynaecologists
The Continence Foundation
307 Hatton Square, 16 Baldwin’s Gardens, London, EC1N7RJ.
Telephone: 020 7404 6875. Fax: 020 7404 6876.
www.continence-foundation.org.uk
Information on Continence service can be found at:
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

