- Reference Number: HEY-597/2018
- Departments: Gynaecology, Oncology (Cancer Services)
- Last Updated: 31 May 2018
Introduction
This leaflet has been produced to give you general information about coming into hospital for your surgery. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What are Enhanced Recovery Programmes?
Enhanced recovery programmes are a national modern approach to ensure a ‘fitter’ patient who will be able to recover faster and return home earlier with fewer complications.
It requires you to be an active participant in your own care. We will focus on improving your pre-operative care which means we will, with the help of your GP, get you in the best physical condition before your operation and also ensure you have appropriate care in place for your discharge home. We would also encourage your relatives/friends to provide support and assistance for you at home.
Whilst in hospital we will reduce your length of stay by admitting you on the day of surgery and use less invasive surgical techniques if possible. After your operation we will manage your recovery (with your participation) with earlier introduction of fluids, diet and mobilisation in order to speed up your rehabilitation.
Our aim is to get you back to full health as soon as possible and research has shown that getting out of bed earlier and starting to eat and drink sooner can help this and reduce any complications. It is important that we work together to help improve your recovery process.
We do need you to assist us to work together to speed up your recovery.
How do I prepare for my admission and surgery?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
Before admission
You will be invited to attend a pre-operative clinic appointment prior to your operation. This appointment is to check how fit your are for surgery, plan your discharge date and give you an opportunity to ask questions about the Enhanced Recovery Programme, your plan of care and your discharge and the care you will require (meals, shopping, social services help, if necessary).
You will be asked about your previous medical and surgical history and as part of your routine care you may have investigations such as:
- Bloods tests
- X-rays
- ECG (heart trace)
- MRSA swabs (to check for infection)
All your results will be checked before your admission for surgery to ensure you are fit for your operation.
If you are currently taking medications it is important that you bring these medications in their original boxes to the pre-operative clinic appointment.
If you take warfarin, aspirin or Hormone Replacement Therapy (HRT) you may need to stop these prior to your operation. Please inform the nurse at your pre-operative appointment if you are taking this type of medication so that you can be advised appropriately.
The appointment will last about 30 minutes hour to one hour depending on the type of surgery you are having and a relative or friend are welcome to join you to support you in planning for your care and recovery.
Anaesthetic Assessment
The nurse will assess your fitness for an anaesthetic initially at the pre-operative clinic and refer you to an anaesthetist if required.
The anaesthetic you receive will depend on you as an individual and may be a general anaesthetic or an epidural.
What we expect from you
Please tell us about your individual needs and circumstances as early as possible. Your length of stay in hospital will vary depending upon the type of surgery you are having. This will be discussed in the pre-operative clinic and then with your nurse on admission. If you have any special requirements, such as social services or transport, please tell your nurse as soon as possible so that they can make the appropriate arrangements for you.
Bowel preparation
Most patients will not require this. If it is required by your surgeon you will be given medicine with instructions on how to take it at home prior to admission.
Fragmin
This is an injection that you may require. It is used to reduce the risk of blood clots developing (see separate information sheet on Venous Thromboembolism (VTE).
Consent
Your consent may be obtained in clinic or on the day of admission. This is always required if you are having an operation or invasive procedure and you may at any time withdraw your consent. Your doctor and anaesthetist will discuss the choices of treatment available to you and recommend an option; you are free to choose another option. You will be asked to sign a consent form and given a copy. The amount of information you require varies with individuals but you should understand what is happening to you and the major risks involved. You are encouraged to ask questions and discuss your concerns and if you do not want certain procedures, please let the staff know. A qualified, experienced doctor will always take consent and explain the procedure to you.
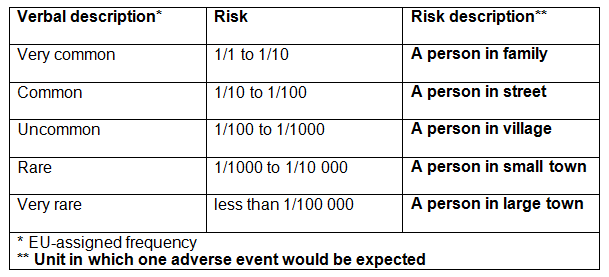
Risks
There is always some degree of risk with any surgery and your doctor and anaesthetist will explain the most common risks of your operation. Remember whether you consent to what is being proposed is your decision. So feel free to ask as many questions as you need and to discuss any concerns fully, whether they are cultural, religious or other. Risk can be described as numbers or words or both. This table may help you to understand how risk is described
Following surgery the doctor will always inform you if something has not gone as planned. However, you may be the first to notice that something is not right. If this happens, tell a healthcare professional right away.
What else do I need to do in the days before coming into hospital?
- Food – We advise you to stock up your freezer and prepare your home ready for discharge. Arrange for family or friends to provide support for you once you are back home.
- Medication – Please ensure you have a stock at home of your usual medications for after your surgery. The ward will not dispense medications that are regularly prescribed by your family doctor (GP).
- Pain relief medication – Also make sure you have a stock of simple pain relief medication such as paracetamol and ibrufen.
- Coughs and Colds – If you have any illness, such as a cough or cold please ring the ward where you are going to be admitted to for advice.
- Shower/Bath – We advise all patients to shower or bath prior to admission but avoid using perfumes, lotions etc. Please note we advise patients to use sanitary towels not tampons for any vaginal bleeding after the operation.
- Smoking – If you are a smoker, it would benefit you greatly to stop smoking or cut down before you have your operation. This will reduce the risk of chest troubles as smoking makes your lungs sensitive to the anaesthetic. If you need further information about stopping smoking please contact:
– Your GP
– The NHS Smoking Helpline on 0800 1690169. A specialist adviser is available everyday from 7am to 11pm
– Hull and East Riding Stop Smoking service on 0800 0915 5959. North East Lincolnshire and North Lincolnshire NHS Stop smoking services on 0845 6032166 (calls charged at local rate).
What should I bring with me into hospital?
Please bring in all medications that you are currently taking. This includes tablets, capsules, liquids, cream and inhalers. Please bring the medications in their original packets so we can easily identify them.
Please leave all valuables at home, including all jewellery, and remove all makeup and nail polish. All personal belongings you do bring in will be your own responsibility as we have very limited storage for any valuables on the ward. Please bring a simple bag including: dressing gown, slippers, wash bag, towel, sanitary towels and night clothes.
There is limited storage on the ward and we aim for a clean, tidy bed area. If necessary, please send unnecessary items home.
If you are on the Enhanced Recovery Programme, we ask you to bring in a set of clothes so you to get dressed throughout the day. These should be easy to put on and take off and be comfortable around your wound site. This is part of aiding a quicker recovery and getting you back to normal as soon as possible.
Before your operation
You will normally be admitted on the day of your surgery unless your surgeon feels you need to come in the day before. Before going to theatre you will be seen by the nursing staff who will prepare you to go to theatre safely. If you have not yet given consent, you will see your surgeon who will obtain your written consent and answer any questions you may have. You will also see the anaesthetist with whom you can discuss pain relief and anaesthetics; this is all to ensure that it is safe to proceed with your surgery. Please inform us if there have been any changes in your details or health since your pre-operative appointment. If you have been asked to come into hospital the day before your surgery, it is possible that you may have to wait for a bed to become available. In this case you will be made comfortable in the day room. Please feel free to ask for food and drinks. If you are coming into hospital on the day of your surgery you will be admitted as soon as possible. You may go straight to theatre from the admissions lounge before being shown to a bed.
We will ask you to put on some tight fitting anti-thrombus stockings. These help to prevent blood clots from developing.
Fasting instructions prior to your operation
You will have been asked not to suck, eat or drink anything prior to your operation (this includes chewing gum or sucking sweets) Your admission letter will inform you the time which you need to stop eating and drinking. It is important to read this. You should have a bath/shower before you come into hospital. You will be given a surgical gown to wear. All make up, nail varnish, false nails and jewellery (except wedding ring), dentures and contact lenses must be removed. You will also need to wear some support stockings to help reduce the risk of blood clotting during the operation. You may need to shave some pubic hair. The nursing staff will advise you or assist you if required.
Following surgery
Day 0 – Immediately after your operation
On returning from theatre onto the ward, it is important to perform deep breathing exercises.
- You will have an oxygen mask on your face.
- You may have an epidural for your pain as well as regular oral pain relief medication.
- If required, you will be given medication to stop you feeling sick.
- You may have a tube in your bladder (catheter) to monitor your urine output.
- You may have a small tube near your wound to remove any excess blood.
- You will be allowed to eat and drink immediately.
- You will have a needle in the back of your hand to give you additional fluids directly into a vein (intravenously).
- Following your operation, we will be checking your blood pressure, pulse and temperature regularly, along with your wound site.
Day 1 – Day after surgery
- You will be seen daily by members of your medical team.
- We will be checking your blood pressure, pulse and temperature regularly, along with your wound site. As part of your mobilisation, you will be asked to sit out bed for up to two hours.
- Your catheter may be removed, this will depend on the type of surgery you had.
- You will continue to eat as normal.
- If you have had a Patient controlled analgesia this may be removed today.
- We recommend you read the physiotherapy information Fit following Surgery:
pogp.csp.org.uk/publications/fit-following-surgery-advice-exercise-following-major-gynaecological-surgery.
Day 2 – Second day after surgery
- Your epidural will be removed.
- You will continue to eat and drink as normal.
- We will be checking your blood pressure, pulse and temperature regularly, along with your wound site.
- You will be required to be out of bed for at least 6 – 8 hours, with rests in between.
- We will confirm your discharge plans.
- You should put on your normal clothes provided you feel well enough, as this has been shown to help patients feel positive about their recovery.
Day 3 – Third day after surgery
- We will expect you to be washing and dressing yourself.
- We will be checking your blood pressure, pulse and temperature regularly, along with your wound site.
- We will liaise with you to arrange transport home.
Depending on your recovery and the date agreed in pre-operative clinic, we will discharge you. If you have had a complication in your recovery or if for any reason your surgeon feels you need to remain in hospital, we will repeat your recovery plan as for Day 2.
You will be expected to continue eating, drinking and mobilising in preparation for going home. Your observations will be monitored and wounds checked. Patients are expected to arrange their own transport home. If you are on benefits you may be eligible to claim travelling expenses. If you require ambulance transport please inform your nurse on admission.
We aim to discharge you from hospital at around 11.00 am but on occasions if your transport/medications, etc, are delayed, it may be necessary to ask you to wait in the discharge lounge.
Day 4 – Fourth day after surgery
If you remain in hospital until day 4/5, your care will continue as on Day 3 until you are discharged. We will be encouraging patients to be independent and self caring as much as possible as part of the recovery programme, however if you have any concerns about your individual care plan please speak to your nurse.
Cancer patients will receive support from our Gynaecology Clinical Nurse Specialist Nurses before and after surgery and can discuss any specific requirements in relation to their cancer diagnosis during admission on the ward, or via their contact line (01482) 624033.
What happens when I go home?
Follow up
If your doctor wishes to see you again they will inform you or your nurse. You will either be given an appointment before discharge or one may be sent to you by post. This may be at your local hospital. Any care required after discharge will be arranged with the community, ward or clinic before you leave hospital.
Abdominal pain
It is quite usual to feel some griping pains (colic) during the first week or so after surgery. The pains should only last for a few minutes and then subside. If you feel continuous abdominal pain that lasts for a few hours, then you should let a doctor know. This could be your GP, or by contacting one of the numbers you have been given.
Wounds
If you require post operative wound care we will arrange for the district nurse to visit you at home. Wounds will usually be closed with dissolvable sutures (stitches). However if non-dissolvable stitches are used this will be discussed with you and arrangements will be made for these to be removed in the community. It is not unusual for wounds to be slightly red and uncomfortable during the first two weeks however please let us know if your wound becomes inflamed, swollen, painful or if it starts discharging fluid. Complications do not happen often but you need to know what to look out for:
- Pain or Fever – If you have severe pain lasting more than 1 – 2 hours which is not relieved with simple pain relief medication or if you develop a fever in the two weeks following your operation, please contact your GP.
- Urine – You should be passing straw coloured urine. If it is darker you may not be drinking enough. If you have any stinging, please ring us as this can be a sign of infection.
- Bowels – It is not necessary to open your bowels before discharge and constipation is common. Make sure you eat regularly, drink plenty of fluids and take regular walks. If constipation lasts more than 3 days, you can take a mild laxative available from your local pharmacy but be sure not to exceed the stated dosage.
Catheter/drain
Depending on your surgery, you may be discharged with a catheter and/or drain in place. If this happens, you will be shown how to care for them prior to going home and you will be given an appointment to return to hospital for follow up. Please do not hesitate to contact the ward if you have any concerns.
Medications
Depending on your surgery, you may be given oral pain relief to take home, along with any other medications your doctor wishes you to have. You will be instructed on how to take any medication and will not have to pay for it. Occasionally, there may be a delay in obtaining the medication from the Pharmacy. We would ask you to be patient or, alternatively, you can arrange to pick it up later if this is more convenient for you.
GP letters/sick notes
Please note that in most occupations you can self certify sick for up to seven days. You do not require a doctor’s sick note; a proof of admission will normally be sufficient. However if you do require a sick note, please inform your nurse on admission and one will be provided. We routinely send your GP a letter informing them of your admission/surgery or management/findings and follow up. Your GP will be able to provide any further sick notes that may be required until you are fit to return to work.
Driving and travel
We advise you not to drive for at least 4 – 6 weeks after your operation. You should only start driving when you can comfortably wear a seatbelt and feel able to make an emergency stop. However it is wise to check with your individual insurance company as they may have different rules.
If you are due to travel abroad shortly after your surgery we advise you to check with your holiday insurance provider prior to travel to ensure you are covered.
Work and exercise
You will be advised on how long you are required to be off work, depending on the type of surgery you have had. The hospital can provide you with a sick note for two weeks. Walking daily is encouraged from day one. You should plan to take regular exercise several times a day. If you are planning to restart an exercise regime such as jogging or swimming, wait two weeks and start gradually. If you are still uncomfortable, modify your exercise.
Sexual intercourse
We advise you to wait six weeks after surgery before resuming penetrative intercourse and to ensure that you have no vaginal bleeding or discharge.
What else do I need to know?
Understanding and managing your pain
Many people are worried about pain and we will do our best to make your experience pain free. When we cannot do this we aim to control your pain to a level that allows you to do the things you need to do to get better, such as walk around, cough, and breathe deeply. These activities help to reduce complications such as bedsores, chest infections and blood clots in your legs.
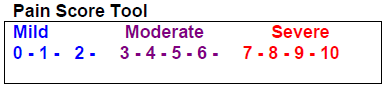
Your nurse will ask you to score your level of pain between 0 – 10, where 0 (zero) indicates you have no pain and 10 represents the worst pain ever; there is no wrong or right answer – only you know the amount of pain you are in. If this method does not suit, please discuss this with your nurse or doctor. Please ask for pain relief medication before it gets too uncomfortable as it is easier to control the pain sooner rather than later, and treating pain will allow for a quicker, more effective recovery.
Pain score tool
There are different ways in which your pain can be managed following your surgery. These include oral pain killers, Patient Controlled Analgesia (PCA) and Epidural:
PCA (Patient Controlled Analgesia)
This is a machine that allows you to deliver a small dose of pain relief medication directly into a vein through a small plastic tube in your hand (cannula). This method gives you greater control of your pain and you will not have to wait for a nurse to help you. The machine has a five minute lockout device so you can not overdose however it is important that no-one presses the button for you.
This option may not completely remove your pain, but your nurse can look at other options to supplement the PCA. Do not wait for the pain to get worse, press the button if you feel pain coming on.
Epidural
A fine tube is put in the spine (epidural space) in theatre by an anaesthetist who then injects local anaesthetic, causing numbness from the waist down. The pump used provides a steady continuous flow of anaesthetic.
This is not suitable for all patients and the anaesthetist will assess your suitability for an epidural prior to surgery. When the epidural is stopped, full feeling will gradually return. An epidural allows an almost painless procedure. At first your legs will feel heavy and difficult to move. When you no longer require this level of pain relief medication the dosage is gradually reduced and then stopped. The sensation in your legs gradually reduces.
Side effects and complications of pain relief medication
With all pain relief medication side effects can occur but all can be treated relatively simply:
- Feeling sick and nauseous is common to all.
- Drowsiness.
- Itching (from morphine based drugs).
- Constipation.
With epidurals other side effects can occur:
- Difficulty passing urine – a catheter may need to be inserted.
- Low blood pressure.
- Backache.
- Headaches.
Rare complications for patients after epidurals can occur. Please inform your doctor or GP if you have: persistent back pain, altered sensation, tingling or weakness in your arms or legs, trouble passing urine or fever along with any of these issues.
Always tell your nurse if you are having problems or the pain relief is inadequate.
What is a venous thromboelism (VTE)?
Venous thrombosis is a condition in which a blood clot forms in the deep veins of the calves, pelvis or thigh. This is also known as a deep vein thrombosis (DVT). An embolism is created if part of the blood clot in the deep vein breaks off and travels through the venous system. This is called Venous Thromboembolism (VTE). The clot will usually lodge in the lung giving rise to a very serious condition called pulmonary embolism (PE).
Who is at risk of having VTE?
VTE can be an inherited problem and there are some medical conditions that will increase the risk of a blood clot. However anyone can develop a VTE and the following can increase the risk:
- Immobility causes the blood flowing in your veins to slow down making a blood clot more likely.
- Surgical operations lasting over 60 minutes when your legs are still.
- Illness or injury causing immobility.
- Long journeys by plane, train or car which requires you to sit in a cramped position.
- Damage to the vein – previous DVT or some chemotherapy drugs that inflame the vein.
- Contraceptive pills and HRT with high doses of oestrogen can also cause the blood to clot more easily.
- People with cancer and heart failure are at increased risk, as are those who are obese, pregnant or over 60.
We assess all our patients on admission to the ward using a national guidance tool to see if you are at an increased risk of developing a VTE. If you are at risk, your nurse and doctor will treat you as necessary.
How can we prevent VTE?
- Avoid long periods of immobility sitting in a chair for many hours. If you can get up and move about regularly.
- Regular exercise of the calves and foot muscles is beneficial.
- Drink plenty of water to avoid dehydration.
- For major surgery of the lower abdomen we will ask you to wear elastic compression stockings.
- We may give you a blood thinning injection (anticoagulant) such as Fragmin.
- We will use inflatable sleeves to compress your legs during your operation.
- We will get you up and about as soon as possible after your operation.
In summary, the main cause of VTE is immobility and we will observe you for any symptoms of tenderness, swelling of the calves, warmth and redness and any breathlessness or chest pain. If you experience any of these symptoms you will require further investigation and treatment, therefore prevention is very important. If you have any further questions please go to the Trust patient information on Venous Thromboembolism (VTE) – Reducing the Risk Department of Health website: www.patient.co.uk/showdoc/23068982.
Infection control – fighting infection together
Hand washing is the most effective way of stopping the spread of germs and bacteria. Always wash your own hands and insist that others wash theirs to protect you.
Alcohol gel dispensers are available at doors and beds. All patients and visitors are asked to use them or wash their hands in the sinks.
Staff – Feel free to ask staff if they have cleaned their hands. They should not be annoyed if you ask them.
Beds – Please do not sit on other patients’ beds or let visitors sit on yours.
MRSA (Methicillin-Resistant Staphylococcus Aureus)
What is it?
Staphylococcus is a bacterium commonly found on skin and in the noses of many healthy people without causing harm. This is known as colonisation. However, it can sometimes cause infections, the most serious being septicaemia (blood poisoning), particularly in those who are already unwell.
Whilst most infections can usually be treated with antibiotics, some strains of Staphylococcus Aureus have become resistant to the usual antibiotics (such as methicillin). These are known as methicillin resistant staphylococcus aureus (MRSA). MRSA is unlikely to present a problem to a healthy person.
How do we reduce the risks?
All patients are swabbed prior to or on admission. Staff maintain good infection control measures, particularly good hand hygiene, as MRSA is most often spread by hand contact. We encourage all staff, patients and relatives to wash and dry their hands when in hospital. Patients with MRSA are usually cared for in a side room to prevent spread and asked to stay within the room and treated with an antiseptic skin cleanser and hair wash. Visitors can come as normal, however, young children and those at high risk are discouraged. No special treatment is required by visitors apart from good hand washing before and after visiting. Treatment is usually stopped when patients are discharged and the patient’s GP is informed. It is important to tell staff if you have ever had MRSA in the past, both for your own safety and that of others.
Diarrhoea or vomiting
If you or your visitors are suffering from any diarrhoea or vomiting, you must inform staff. Friends or relatives with infections must refrain from visiting to protect other vulnerable patients from the spread of disease. They should not visit until they have been symptom – free for at least 48 hours.
Visitors
Ward visiting hours – Please check with the ward for their visiting times.
You may bring a partner/friend on admission to provide support before theatre but they will be asked to leave when you are admitted onto the ward.
Please respect that most of our patients will have under gone surgery so will need quiet time to recover. Visitors should be kept to a maximum of two at any one time.
It is also advisable not to bring children to visit unless this has been agreed beforehand with the ward manager and it is felt to be in the child’s best interest.
Chaplaincy – Multi-faith spiritual care
The Trust has its own Chaplaincy service. Some people find that a visit from a Chaplain is helpful whilst they are in hospital.
Step by step guide to recovery
It is important to take enough rest, however you should start some of your normal daily activities when you get home and do more slowly.
Step 1: Day 1 – 4 after leaving hospital
- No domestic chores whatsoever. Lie down for at least one hour a day.
- Listen to your body/mind/spirit – if you want to go to sleep then do so for you will have less energy than you thought.
- No stretching or lifting anything heavier than a kettle with water in it for one cup/mug full.
- Try to maintain your gentle mobility exercises.
- Enjoy a daily bath/shower.
- Go to bed early.
Step 2: Day 5 – 7 after leaving hospital
- Lie down for at least one hour a day.
- Help with washing up and or dusting but avoid stretching or lifting.
- Go for a five minute walk.
- Try to maintain your gentle mobility exercises.
- It is important to rest as needed
Step 3: Weeks 2 – 3 after leaving hospital
- Gradually increase walking. Stop if you feel tired.
- Decrease the rest period rather than resting most of the time and being occasionally active.
- Light shopping.
- No lifting of shopping, suitcases, furniture, full saucepans.
- Try to maintain your gentle mobility exercises.
- It is important to rest as needed.
Step 4: Week 3 – 4 after leaving hospital
- Start moderate activity – going to the shops and some light shopping.
- Help with washing up and/or dusting.
- Rest if you feel tired.
- No lifting of shopping, suitcases, furniture, full saucepans.
Step 5: Weeks 5 – 6 after leaving hospital
- Light house work such as vacuuming in an upright position.
- Driving a car is possible, providing you have checked with your insurance company and can do an emergency stop.
- Listen to your body/ mind/ spirit if it feels tired then rest.
Useful contacts
Should you require further advice please contact: Gynaecology Outpatients, Women and Children’s Hospital – (01482) 607829.
Women’s Health Outpatients, Castle Hill Hospital – (01482) 624045.
The Gynaecology Oncology Clinical Nurse Specialists are happy to speak to you at any time. If they are not there an answer phone is available on (01482) 624033.
Information on Gynaecology Services at Hull University Teaching Hospitals NHS Trust NHS Trust: www.hey.nhs.uk/gynaecology.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.