- Reference Number: HEY-428/2023
- Departments: Tissue Viability
- Last Updated: 31 March 2023
Introduction
To help prevent pressure ulcers it is important that we work together to prevent unnecessary deterioration of you or your friend/relatives skin. Hull University teaching hospitals use the aSSKINg care bundle –a nationally recognised tool to prevent pressure ulcers.
A-Assessment
S-skin inspection
S-surface selection-mattress or seat cushion
K-keep moving
I-Incontinence management
N-Nutrition
G-Give information
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a pressure ulcer?
A Pressure ulcer is an area of damage to the skin and underlying tissue, commonly known as bed sores. They are usually caused by sitting or lying in one position without moving over a period of time. A pressure ulcer can develop very quickly even in a few hours, especially if you are unwell.
Pain is one of the first signs that a pressure ulcer may be developing and your skin will start to change colour. It may appear slightly red or darker in colour than usual and does not fade when pressure is removed. In some cases it can appear purple /maroon in colour and can initially be mistaken as a bruise .
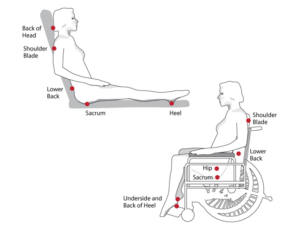
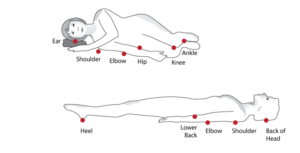
In people who have darker skin tones it is not easy to detect a reddened /purple area. In this case, it is best to check by touching the areas of the body that are at risk from pressure ulcers –see diagram. These areas may feel warmer or cooler to touch, firmer, spongy or swollen.
Your help in detecting the early signs of skin damage is important to alert our staff to help prevent pressure ulcers developing or getting worse.
If the early signs of a pressure ulcer are not treated quickly, it can develop into an open wound, which can lead to a more serious pressure ulcer. If you notice any signs of pressure damage, please notify a member of our staff immediately.
If you already have early signs of a pressure ulcer or have one already, you will be provided with the appropriate pressure relieving mattress. Within our trust we have different types of mattresses and cushions which will help reduce the pressure off your skin. All of our foam mattresses are made of high quality foam but if you need a more specialised mattress or cushion, the staff will assess you for this.
Self-care
- Keep your skin clean and dry, including under your breasts, in between the cheeks of your bottom, under your scrotum.
- Moisturise your skin.
- Co-operate with any moving and turning programme we plan for you.
- Your pressure ulcer may need other treatments to help it to This could include dressings and referrals to other health professionals.
- Ask your health care professional if you are unsure of any aspect of this care.
Are you at risk of developing a Pressure ulcer?
Anyone can develop a pressure ulcer but some people are more likely to develop a pressure ulcer than others.
You are at risk of developing a pressure ulcer if you:
- Are not eating a balanced diet or having enough to drink
- Have to stay in bed for a period of time
- Have problems moving position without help
- Are in a wheelchair
- Spend a long time in an armchair or on a sofa
- Are seriously ill (even for a short period of time)
- Are undergoing surgery
- Are incontinent
- Have lost your feeling in part(s) of your body (e.g. after a stroke or spinal cord damage)
- Have poor circulation
- Have previously had a pressure ulcer
- Pain preventing movement / hindering re positioning
- Have medical devices in place
- If you are taking multiple medications
- Unwell and less mobile requiring hospital admission
Unfortunately pressure ulcers can develop very quickly in frail elderly people. Damage may not involve just the skin but also deeper into the tissues beneath.
Pressure ulcers can be painful and you are more likely to develop an infection which can then make you seriously ill. They can take a very long time to heal and can delay your discharge home. This will allow us to monitor if it is improving or getting worse, in which case we will suggest a change in treatment. This may be by increasing the frequency of turns, a di
If you are in bed:
- Change your position, regularly alternate between your back and sides. This may be difficult for you to do on your own and a nurse will help you. It is important that you remind your health and social care provider that you need to be turned. Please help us by you or your carer reminding us that you need to be turned.
- If you have red/blistered heels we may need to raise your feet off the bed.
- If you are sitting out of bed but cannot move yourself around or stand up, it is important that you do not sit out of bed for more than one hour at a time. Our staff will assist you if you need help to get back into bed.
If you are in a wheelchair
- Try to take your weight off your bottom every half an hour by leaning to one side or pushing up on the arms of your chair.
- Regularly roll from buttock to buttock a few times every half an hour.
- You should not sit in your wheelchair for more than two hours at a time, even with a specialised cushion.
What else can you do to help prevent pressure ulcers?
Eat a healthy diet and drink plenty of fluids, if this is possible .We may refer you to a dietician and provide supplements.
Inform our staff of any equipment to prevent or treat pressure ulcers you already use.
Which areas of skin are most at risk?
The common places for pressure ulcers to occur are on parts of the body that take your weight and where bone is near to the surface of the skin. For example, bottom, heels, hips, elbows, ankles, shoulders, spine and the back of the head.
Devices in use to support your care may also cause damage to the skin from pressure if not repositioned regularly.
If you have any questions regarding your pressure ulcer risk, care planned or equipment used please ask your health care professional.
To ensure your care is planned as required the nursing staff will seek your permission to check your skin to ensure no damage has developed or that your skin is not more vulnerable than usual. This leaflet is aimed at providing you with the information to support why this is necessary.
This leaflet was produced by the Tissue Viability Team, Hull University Teaching Hospitals NHS Trust and will be reviewed in April 2026
Ref: HEY-428/2023
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

