- Reference Number: HEY214-2024
- Departments: Endoscopy, Upper GI Endoscopy
- Last Updated: 1 April 2024
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
Please ensure you read the full leaflet before coming for your endoscopy.
What is an Upper GI Endoscopy?
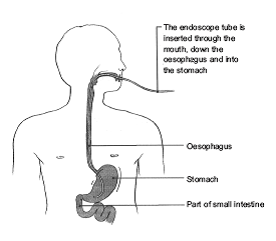
You have probably been troubled by some symptoms and is why your doctor has advised an Upper GI Endoscopy. This is a test that allows the endoscopist to look directly at the lining of the gullet (oesophagus), stomach and first part of the small intestine (duodenum) – see diagram below.
A slim flexible tube with a light on the end is gently passed from your mouth into your stomach. Pictures from the tube are shown on a TV monitor and a clear view of your gullet, stomach and duodenum can be seen. A small sample of tissue (biopsy) can be taken for analysis in the laboratory. This is removed painlessly with a tiny pair of forceps. Other names used for an Upper GI Endoscopy that you may hear are Oesophagogastroduodenoscopy (OGD) and Gastroscopy.
Pictures used with the kind permission of Health Press Limited from Neild P, Gazzard B. Patient Pictures – Gastroenterology, Oxford Health Press, 1997
Can there be any complications or risks?
If you have any known allergies or reactions to any medications, please let the endoscopist and your nurse know.
Common problems that are not serious can include a sore throat, bloating. If you choose to have sedation you may experience bruising from the needle used to insert the cannula into your hand/arm.
All endoscopies carry a very small risk of bleeding or perforation (a small hole being made) of the bowel, stomach or gut. If this occurs, you will need to be admitted to hospital as sometimes an operation is needed.
There is a possibility of developing aspiration pneumonia (a lung infection that can develop if you inhale food, liquid or vomit into your lungs). There is also a slight risk of damage to crowned teeth or dental bridgework.
If you would like to know more, please ask your nurse or endoscopist.
Are there any alternatives to this test?
Yes, an X-ray examination including a barium meal can be undertaken, which can often tell us if the area looks abnormal or not but cannot always tell us what the problem is.
What if I refuse to have the Upper GI endoscopy?
It is your choice whether or not you have the procedure. However, this procedure can provide important information about your gastrointestinal tract, help us to understand your symptoms and plan your treatment.
Please discuss this with your doctor and specialist team.
Who will do my test?
A consultant, senior doctor or specialist nurse (who is trained and experienced in performing the test) may undertake this for you.
Doctors and/or nurses who are undertaking endoscopy training may perform your procedure. An experienced endoscopist will supervise them. Your permission will be requested in advance for this. You may decline and the supervising endoscopist will perform the endoscopy.
Where will the test be performed?
An Upper GI endoscopy is usually performed in the Endoscopy Department at Hull Royal Infirmary or Castle Hill Hospital depending on where your consultant is based. Please make sure that you go to the correct Endoscopy Department. Directions will be given with your appointment letter.
How do I prepare for the test?
- Please read this information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination. Complete the health questionnaire as fully as possible and bring it with you.
- To ensure we have clear views of your stomach, stop eating food 6 hours before your procedure. You can drink water up until 4 hours before your procedure. Do not eat or drink anything during the 4 hours leading up to your procedure.
- If you take any of the following blood thinning tablets please contact the Endoscopy Department before your appointment for further advice: Warfarin, Apixaban, Rivaroxaban, Dabigatran, Argatroban, or Edoxaban.
- Clopidogrel (Plavix) – Please inform the Endoscopy Department if you are taking these tablets as these may need to be stopped prior to your procedure.
- Do take any other regular medicines up to 4 hours before. Contact the department if you are unsure.
- If you have diabetes or a serious heart, lung or kidney problem, or are concerned that a health problem you have may be affected, please contact the Endoscopy Department where you are having your examination (see contact numbers below).
- Pregnancy – It is important that you inform us if there is a possibility that you may be pregnant. Any information you share with us will be kept strictly confidential.
- Latex – Please inform the Endoscopy Department if you have a confirmed latex allergy as this will affect your appointment time.
- Creutzfeldt-Jakob disease/variant Creutzfeldt-Jakob disease (CJD/vCJD also known as Mad Cows Disease) Please inform the Endoscopy Department if you have been notified that you are at risk of CJD/vCJD for public health reasons.
What happens to me in the Endoscopy Department?
Upon arrival
A nurse will collect you from the waiting room and explain what will happen next. You will be given an approximate time of when you may be collected to go home. It is advisable to leave any valuables at home.
Occasionally there may be a delay in your appointment time, due to an emergency taking place. If there are any delays you will be notified as soon as possible and be kept informed.
Health Questionnaire
We will ask you questions about your general health and work through the health questionnaire you have completed for us. Please feel free to ask questions.
Consent
The endoscopist or someone trained in taking consent will meet you and explain the test to you. You will both sign a consent form. This is to confirm that you understand what will happen and agree to the procedure being performed. If you have any questions or worries, please tell us.
In the Procedure Room
We will check your blood pressure, pulse and oxygen levels, before your test. If you wear glasses or dentures, you will be asked to remove them.
You will be given a local anaesthetic throat spray or sedation. You will be made comfortable on a trolley on your left-hand side as this is the best position for the procedure. If you have any problems lying on your left hand side please inform a member of the team.
To keep your mouth open, a plastic mouth guard will be placed between your teeth. A fine plastic tube will rest by your nostrils to give you some extra oxygen. A probe will be placed on your finger to monitor your oxygen levels and pulse rate. If you are having sedation, it will be given at this time and you will feel relaxed and light-headed.
Recovery Area
If you have had throat spray, you will be able to get up as soon as you feel ready and have a cold drink. You do not require someone to stay with you for the next 24 hours.
If you have had sedation, you will need to rest in the recovery room for approximately 30 minutes. You will then be helped to a chair and given a drink. Your relative or friend will then be contacted to collect you.
Sedation
Most people do not require sedation and have the test with their throat numbed by a local anaesthetic spray. The advantages of not having sedation are:
- It is the safest way to have the test
- No long lasting drowsy effects for the day
- You can return to all normal activities (including driving) as soon as you wish
- You do not need someone to take you home or stay with you
- You will be able to understand any results, advice, or instructions
However, some people do require sedation. If you think you will require sedation please discuss this with the nurse when you arrive.
Other rare complications include a reaction to the sedation drugs. Some people are particularly sensitive to these drugs. Your breathing can become too shallow and too slow. In these cases we stop the examination, give more oxygen and if required we can give a drug that reverses the effect of the sedation. This is usually all that is needed and the person normally recovers with no ill or lasting effects.
The sedation drugs may cause difficulty in breathing for people who have heart disease, unstable angina, severe asthma, chronic bronchitis or have had a stroke. 70 patients out of 100 having sedation experience a drop in oxygen levels and therefore we monitor your breathing and heartbeat throughout and give oxygen by nasal tubes.
Sedation is given through a small plastic tube called a cannula in the back of your hand or in your arm. A needle is used to insert this but removed as soon as the cannula is in place. The sedation makes you feel relaxed but does not normally ‘put you to sleep’. You can still respond to what is happening.
It is very important that you have someone with you after sedation as it can have effects that last up to 24 hours after the test. You can become forgetful and also sleepy again.
Your test may be cancelled if you do not arrange to have someone to collect you and stay with you for the next 24 hours if you require sedation.
We strongly recommend that for the next 24 hours you:
- Do not drive
- Do not return to work or operate machinery
- Do not sign any important or legal documents
- Are not left alone, you may be at risk of injuring yourself
- Are not left alone to care for children
If you are an outpatient, the person accompanying you will be contacted to collect you. If you are an inpatient you will be transferred back to your ward.
What will the test feel like?
You may feel the tube gently slide over your tongue and down your gullet; you may feel it move around in your stomach. It will not interfere with your breathing but it can be uncomfortable. Some air will be passed down the tube to inflate your stomach to allow a clear view. If you get a lot of saliva, the nurse will clear it with suction like at the dentist. The test normally takes five minutes or less.
During the procedure you can help by listening to the instructions your nurse gives you. By staying calm and relaxed, the test goes quickly and easily. Try to control your breathing by taking slow deep breaths. This helps stop you wanting to retch.
At any point during the procedure you can withdraw your consent and ask for the procedure to stop. If this happens the endoscopist will stop the test and take the scope out.
What happens when the test is finished?
It is quite likely that the back of your throat will feel sore for the rest of the day. You may feel bloated if some air remains in your stomach. Both discomforts usually pass without any medication; you may find it helpful to eat light meals for the next 24 hours.
The recovery nurse will explain your test results to you and (if you wish) the results will be told to your carer as well. These will be written on your discharge form with any instructions that you need to follow. Your hospital doctor and your doctor will receive a copy of the results. Results from a biopsy may take up to 4 to 6 weeks to reach your doctor.
Further information:
If you require further information about your test your doctor, consultant and the Endoscopy Department are valuable sources.
Useful contact numbers:
- The Endoscopy Department, Castle Hill Hospital, tel: 01482 622069 (direct line), Monday to Friday from 8.00am to 5.00pm
- The Endoscopy Department, Hull Royal Infirmary: tel: 01482 674790, Monday to Friday from 8.00am to 5.00pm
- Ward 100 Hull Royal Infirmary – Out of hours, tel: 01482 674860
You will be given an Upper GI Endscopy Information Checklist to complete as part of the consent for your procedure – please see the link:
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

