- Reference Number: HEY-380/2020
- Departments: Orthopaedics
- Last Updated: 30 June 2020
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a total hip replacement?
The operation
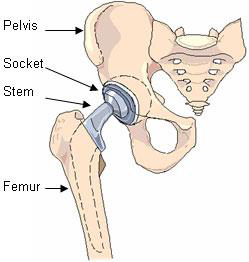
The surgery removes the worn and eroded cartilage (arthritis), together with the top of the femur (the “ball” of the ball-and-socket joint), and replaces it with components made of metal/polyethylene/ceramic. These components may or may not be fixed with bone cement (depending on the design used).
The operation takes around one to two hours but you will be in the theatre department for longer, to allow you to recover from the anaesthetic.
Why do I need a total hip replacement?
You have been offered a hip replacement for the pain you have in your hip, as other methods of improving it have not succeeded (pain relief, anti-inflammatory tablets, exercise, walking stick etc.). This leaflet is intended to help you reach a decision by outlining the operation, risks, benefits and outcome of a hip replacement. The content of this leaflet is not intended to be a comprehensive list or replace the discussion between you and the surgeon or your doctor, but rather is a brief guidance to the degree of benefit and risk which you need to consider.
Can there be any complications or risks?
Following surgery, the pain and stiffness from your hip should gradually improve. The majority of patients are able to increase their activity over time (months).
Most patients who have a hip replacement are very happy with the results and are glad that they have had it done. A minority (5%) have lingering symptoms or are unhappy with the outcome for a variety of reasons, particularly if a complication has occurred. In addition, smokers, overweight patients or patients with pre-existing medical conditions like diabetes, high blood pressure, high cholesterol, previous heart attack or stroke will have an increased risk of complications. We try to decrease these risks by optimising your condition prior to surgery with the help of your doctor, other specialists and the pre-assessment clinic, but we cannot eliminate them.
Risks of a Total Hip Replacement
The Risk |
What Is It And What Is Done About Decreasing Or Managing It |
| Clots in legs/lungs DVT/PE (Thrombosis) | Leg clots happen in half of patients unless precautions are taken e.g. use of special stockings, pumps and medication (which we do). They can still happen (much less often), even if these measures are used. Clots in legs can travel to the lungs in 1 – 2% of patients and can lead to death in 1 in 3000. Moreover, 5% will get pain and swelling in the legs. |
| Strokes, heart attack or heart failure | These do happen without surgery; there is nothing to stop them happening while you are in the hospital although the stress of surgery can increase the chance of such an event. |
| Nerve or Blood vessel damage | As a result of surgery you should expect numbness to a varying degree around your hip. This is because the surgery involves cutting the small skin nerves around the wound. More rarely, the blood vessels (0.1%), or the nerves (1%) which allow you to feel or move your leg, may get damaged, resulting in discolouration of your whole leg, changes/disturbance in the temperature of your leg, weakness of your leg/foot (possibly including foot drop, where you are unable to pull up your foot at the ankle) or severe numbness. These problems will usually recover, but occasionally do not. In extreme cases, damage to the nerves or vessels may lead to death. |
| Bone breakage | This can occur at any time, or during surgery, depending on your bone strength. Fractures occurring during surgery can usually be repaired (if needed) during the same operation (sometimes using a different design of replacement) but the return to mobility may need to be taken more slowly. |
| Infection | Wound infection is decreased by giving you antibiotics at the time of surgery and immediately after. If it occurs, it can be superficial (2 in 100 – easier to treat) or deep (6 in 1000, more difficult to treat). Infection can occur at any time after surgery (days or years) and can lead to the hip replacement failing. If this happens, you might need further surgery such as revision replacement. In extreme cases, infection can result in death. Infection can also occur in your chest or urinary tract (water works), which could lead to infection spreading to your hip. |
| Dislocation | Hip replacements can dislocate (approx. 4%). This can happen if you fall; it can happen if you put your leg into an awkward position. It is very important for you to follow the advice of the physiotherapists in order to minimise this risk. If the hip does dislocate you will need to return to hospital for it to be put back. Occasionally this becomes a recurrent problem needing further surgery (which even then may not be successful). |
| Leg length difference | Whilst your legs will normally be about the same length following hip replacement there can sometimes be a difference which you notice. This may mean needing to have either an insert in, or a build-up on, one or other shoe. |
| Wear/ loosening | With time the hip might wear out and you might require another hip (revision), which may not last or be as good as this one for many reasons. We do know however that at least 85% of hip replacements are still working well 20 years after they are inserted. |
| Residual symptoms | Although most patients are free of pain following hip replacement it is not the same as having a normal hip again. You may notice aching after activity. |
How do I prepare for the total hip replacement?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
Should I have the operation?
If you do not wish to have a hip replacement, you do not have to. It is an individual decision which you make depending on how bad your pain is, how much it disrupts your life style and how much you can put up with. Your arthritis and your symptoms are likely to get worse with time, but they may not. Use of pain relief and / or anti-inflammatory medication usually helps. Walking aids can help mobility. Keeping your weight within the normal range will help in controlling your symptoms.
If you choose not to have an operation at this stage you can always have it later when you feel that your condition warrants it.
What will happen?
Before admission (usually about 2-3 weeks) you will receive an appointment for pre-assessment. This takes place at Castle Hill Hospital. You will have a series of tests and a nurse will discuss your admission and any particular needs you might have. You will also receive physiotherapy advice on recovering your mobility, often involving a separate class.
You may be asked whether you agree to donate the bone which is routinely removed at operation to the Bone Bank, rather than it being disposed of. We are licensed to store bone for it to be used later when needed, e.g. for revision surgery. This involves some additional blood tests and is entirely optional; the Bone Bank does support our patients needing complex surgery and it would be very helpful if you would agree, if asked.
If any medical problems arise between pre-assessment and admission, please contact the ward to check that surgery can still go ahead; for example if you are unwell or if any skin problems arise (e.g cuts, spots etc).
Regarding admission, most patients are admitted on the day of surgery but a few are admitted on the evening before. The surgery takes place at Castle Hill Hospital – your ward will be shown on your admission letter. Please take particular note of instructions in the letter regarding the latest time you can eat or drink before surgery; this is very important.
The surgeon and anaesthetist will visit you before the operation. The anaesthetist will discuss possible options, which may include regional or general anaesthesia, together with post-operative pain management. We recommend regional (spinal) anaesthesia, unless due to medical reasons, as it tends to lead to a quicker recovery after the operation.
What happens afterwards?
Recovery from surgery
It is well known that if patients have a shorter stay in hospital, they are less likely to suffer complications such as infection and blood clots. For that reason we encourage you to get out of bed and discharged home, as soon as possible. This involves a programme known as Enhanced Recovery after Surgery. It is an intensive programme of rehabilitation, with assistance from the physiotherapists and occupational therapists, aiming to keep the time that you need to stay in hospital to a minimum – usually 2 to 4 days, depending on many factors (age, how well motivated you are, physiotherapy etc).
A target discharge date will be set when you are admitted and we are all aiming to achieve this for you. You will not be allowed to go home until you are safe and the physiotherapist is satisfied. For this reason you will not usually need to see a physiotherapist again after you go home, although it is necessary to work on your exercises (as shown) for several months.
You should expect to have some pain at the operation site. To help this we may give you an injection in your spine or to the nerves next to the spine, or patient controlled analgesia, which is when pressing a button gives you pain relief; or we may choose another method of controlling your pain. We will do our best to control your pain as much as possible without endangering you, if necessary involving a dedicated pain management nurse. Further details will be available to you in the pre-assessment clinic.
The majority (around 95%) of patients who have a hip replacement are very pleased with the outcome and are glad that they had it done, even if they have some residual aches in their leg. They feel that the surgery has improved their quality of life, even if it has not necessarily cured all their symptoms. A minority (5%) will have had a complication of some type, the degree of which will affect their outcome/ benefit from the operation, or they may have significant ongoing symptoms.
There are things which you should expect following hip replacement surgery. These include: numbness around the hip; swelling of the leg for several months, bruising in the early weeks after surgery, residual aches in the leg or hip (in some cases for unknown reasons); possible back pain and/or trapped nerve symptoms, particularly if these were present before the operation.
Looking after your new hip
- Avoid gaining weight.
- Be careful in slippery conditions or uneven areas to avoid falls.
- Regular walks will help keep you mobile.
- See your doctor for possible use of antibiotics before dental or medical procedures
- See your doctor for early treatment if you develop chest or urinary tract infection.
Please do not hesitate to discuss the operation with your surgeon, members of the team, your own doctor or friends before making your final decision. Remember that you can always change your mind and pull out of having an operation without offering an explanation.
This leaflet is not intended as a reference to the operation but informs you of some of the issues. For more information you can look at the following web sites/addresses:
www.nhs.uk/Conditions/Hip-replacement/Pages/Introduction.aspx
https://www.britishhipsociety.com/uploaded/BHS%20Hip%20Replacement%20Info%20Booklet.pdf
http://www.arthritisresearchuk.org/arthritis-information/surgery/hip-replacement-surgery.aspx
http://orthoinfo.aaos.org/topic.cfm?topic=A00213
http://orthoinfo.aaos.org/topic.cfm?topic=A00377
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Orthopaedic Department, via your consultant’s secretary (01482) 328541.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

