- Reference Number: HEY-750/2016
- Departments: Elderly Medicine, Nutrition Support
- Last Updated: 17 March 2016
Introduction
This leaflet has been produced to give you general information about your family member and some of the eating and drinking difficulties they may experience as a result of having dementia. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the Speech and Language Therapist, but may act as a starting point for discussion.
If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team. If you have any further concerns about their eating and drinking once they have been discharged from the hospital then you will need to contact their GP.
Nutrition
Many older people do not eat enough to maintain good nutrition and often report a reduced appetite. One of the symptoms of dementia as the disease progresses is a reduction in appetite and satiety (the absence of hunger).
Poor nutrition can lead to a host of problems including:
- The breakdown of tissue e.g. their skin may be frail and they could be prone to pressure ulcers.
- Poor wound healing.
- Weakness and poor mobility.
- Memory loss and disorientation.
Poor nutrition can also impair a person’s ability to swallow (dysphagia), especially if the person is very frail. However there are certain things that may help.
What is Dysphagia?
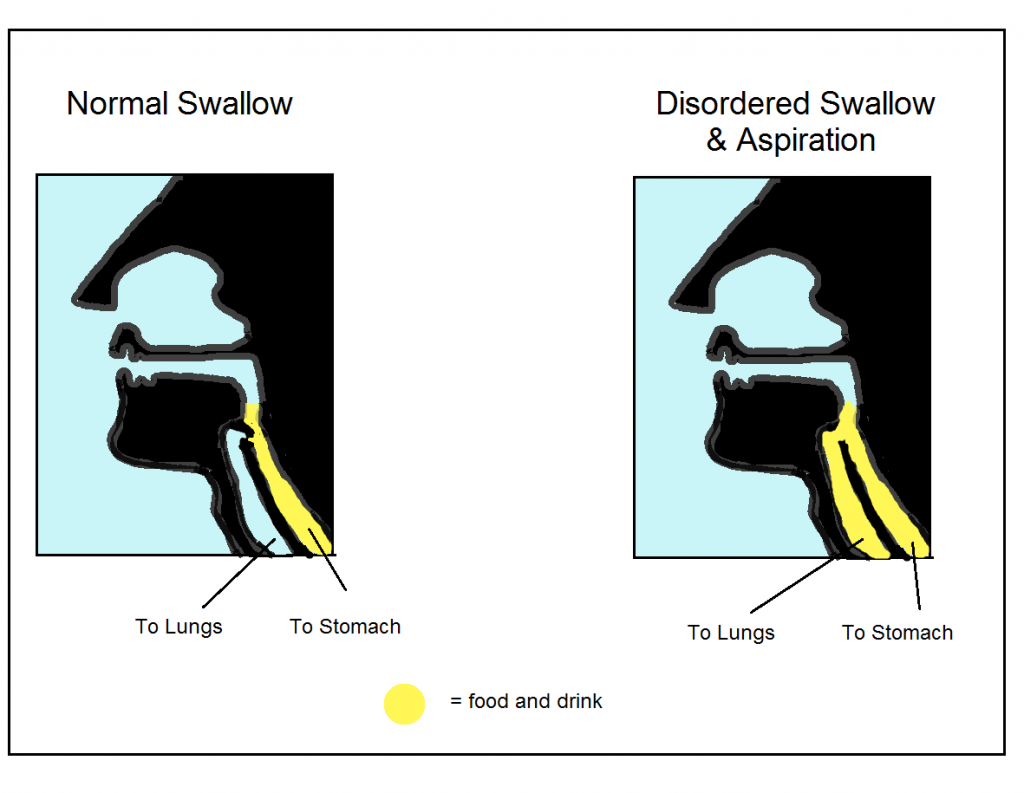
- Dysphagia is a swallowing difficulty. It is very common for individuals with dementia to have difficulties with feeding, eating, drinking and swallowing.
- Problems with swallowing can be as a result of changes that occur in the brain as well as environmental challenges (e.g. a noisy dining room).
- There are risks associated with having dysphagia including aspiration (food going down the wrong way into the lungs), choking, poor nutrition and a reduced quality of life.
Signs that someone may have Dysphagia
- Difficulty chewing and moving food to back of mouth.
- Wet or gurgly voice during and/or after swallowing.
- Coughing whilst eating and drinking.
- Chestiness or recurrent chest infections.
Eating and drinking difficulties in Dementia
- Forgetting to put the food into their mouth, forgetting to chew or swallow it and talking with mouth full.
- May repeatedly chew and not swallow the food.
- Leave most of their meals.
- Physical difficulties chewing certain foods.
- Overfilling their mouth and eating quickly.
- Poor coordination of swallow – food may go down the wrong way.
- Worry that they have not ‘paid’ for their food.
- Believe that the food is poisoned.
- Not recognising the food as something edible.
- Getting tired and giving up eating.
- Spitting out lumps.
- Difficulty swallowing tablets.
Advice on how you can help
Environment
- People with dementia rely on guidance from others – eating with others is important. That is why having a dining companion or a family member to encourage them to eat more is helpful.
- Try and create a relaxed and comfortable environment for the person to put them at ease.
- Use contrasting coloured plates and cutlery so they can see their food.
- Familiar dining space using own tablecloth and cup often relaxes the person and may encourage them to eat more.
Before eating and drinking
- Respect their food and drink preferences, may need assistance with choosing their meals.
- If you are concerned about their nutrition you can ask the nurse about what extra snacks are available and if a dietitian is required.
- Sit at their eye level if they require assistance with feeding. Try experimenting with strong/different tasting foods (sweet/sour/spicy etc) explore what they really enjoy.
- You may need to offer little amounts of food, often (e.g. snacks/ finger foods to be offered or available at any time).
- Provide high calorie foods.
During eating and drinking
- Staying with the person throughout the meal and assist by gradually supporting them, with the ultimate aim to encourage complete independence e.g. consider starting the person off then phasing out assistance.
- Try offering an empty cup/spoon to prompt a swallow.
- Prompt or model eating behaviours as well as giving verbal prompts (e.g. prompt to swallow, gesture chewing).
- Talk about the smell/taste of the food; use a gentle tone of voice.
- Try not to rush them.
The Butterfly Scheme
The Butterfly Scheme at Hull University Teaching Hospitals NHS Trust is used to easily identify people with dementia, in order to support them in the best possible way.
- With the patient’s consent, or if deemed in their best interest (if they are unable to consent), a symbol of a butterfly is placed above the patient’s bed so that staff can offer specific support.
- A carer sheet is placed at the end of the bed and with the family’s support, personal information is collected so that the specific needs of the patient are identified and met.
- The Butterfly Scheme provides all staff with training to enhance their skills in helping people who have dementia.
Contact Details
Other information may be found at www.alzheimers.org.uk
If you are concerned about a family members swallowing, please contact their GP
Should you require further eating, drinking or swallowing advice, please do not hesitate to contact the Speech & Language Therapy Department Telephone number: (01482) 604331.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

