- Reference Number: HEY-390/2020
- Departments: Gynaecology, Oncology (Cancer Services)
- Last Updated: 27 February 2020
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is surgery for a pelvic mass and what does it involve?
Surgery for pelvic mass is performed following the results of investigations (e.g. scans) or a discussion with your consultant. This type of operation is called a laparotomy. This involves cutting the abdomen, starting at the top of the pubic hairline and going up to and sometimes beyond the belly button in an up and down cut.
Why do I need surgery for pelvic mass?
This operation is to find out the cause of your pelvic mass (this may have been called a cyst, lump or growth). After the operation this will be sent for testing.
This operation could also be as part of your treatment for a confirmed ovarian cancer, fallopian tube or primary peritoneal cancer (peritoneum is the membrane which lines the inside of the abdomen). This surgery is called interval debulking surgery (IDS).
The extent of the surgery depends on how concerned the doctor is about the risk of cancer and on how much the cancer, if present, has spread. If cancer is found, as much of the tumour as possible is removed, in some cases it is only possible to remove a small amount.
The operation depends on what is found. Usually it will involve removal of both ovaries and fallopian tubes and womb (hysterectomy). Often we also remove the omentum – this is a pad of fat that is attached to part of the large intestine, and is a common place for cancer to spread to.
This type of cancer may sometimes require bowel surgery. The doctor may have to form a stoma by bringing part of the intestine out onto the surface of the abdomen to allow you to have your bowels open into a bag. Although most patients do not require this extra type of surgery, your individual risk will be discussed with you by your consultant.
Can there by any complications or risks?
All operations requiring a general anaesthetic carry with them a small chance of complication. Every care is taken to keep the risks as low as possible.
The potential complications include:
Infection – The risk of post operative infections is reduced by giving “preventative” antibiotics around the time of surgery, but can still sometimes occur in the pelvis, bladder, chest or in the wound. Infections are usually easily treated with antibiotics. Occasionally an abscess may form (this is a collection of pus) which may require surgical drainage under anaesthetic.
Bleeding – This may occur during the operation or rarely afterwards, and you may require a blood transfusion during your operation. Occasionally if blood collects in the abdomen it may need to be drained under anaesthetic.
Injury to your bladder – This can happen during your operation, because the bladder is close to where the surgery is being performed. You may experience problems passing urine after your operation and it may be necessary to have a catheter put back into your bladder. This may only be for a few days but sometimes may be longer.
Deep vein thrombosis and pulmonary embolism – It is possible for clots of blood to form in the deep veins of the legs and pelvis. This is called a deep vein thrombosis (DVT). It will normally cause pain and swelling in the legs and can be treated relatively simply with drugs. However, in rare cases, it is possible for a clot to break away and be deposited in the lungs or heart. If this occurs it is a serious situation. The risk of developing a DVT is low, as many precautions are taken to help reduce the risks. Moving around as soon as possible after your operation can help to prevent this. We will give you surgical compression stockings to wear whilst you are in hospital, and injections to thin the blood. See patient information on Venous Thromboembolism (VTE) – Reducing the Risk.
Injury to your ureters – Very rarely occurs. The ureters are the tubes that connect your kidneys to your bladder. It is possible for them to be injured during surgery and further surgery may be necessary to repair this.
Bowel injuries – Your bowels share the same cavity as your womb and ovaries and they can occasionally be damaged during this surgery. This is especially so if there is any scar tissue or cancer attached to them. Whilst this problem can normally be easily repaired, it is very occasionally necessary to form a stoma by bringing part of the intestine out onto the surface of the abdomen (colostomy).
Are there any long-term complications? – The skin around the wound is usually numb for several months. This usually improves within 6 – 12 months. This is due to nerves healing and reconnecting back after surgery.
How do I prepare for my operation?
Share the information it contains with your family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following your operation.
What will happen?
It is important to keep your wound clean. A daily bath or shower is advisable paying particular attention to the genital area and the area around the wound. Avoid the use of highly scented soaps, bubble bath and vaginal deodorants etc. Your wound dressing will be looked at daily. You will have stitches or staples in your wound. These will be removed 10 days after your operation. Sometimes the stitches are dissolvable and do not need to be removed.
Most patients stay in hospital for 3 – 5 days after the operation.
What happens after your surgery?
For more information about what happens after your surgery, please read the Gynaecology Enhanced Recovery information for patients.
When will I get my results?
Following your operation the mass (cyst, lump or growth) will be sent for testing. The test results will not be available before you are discharged home. At about 3 weeks after your operation an appointment for an outpatient clinic will be made to discuss the results, and any further treatment options if necessary. This may be at your local hospital.
If you do have cancer, then you may need further treatment. We will discuss this in detail with you if it is necessary. You may need to attend for regular follow-up appointments once your treatment is complete.
If you have interval debulking surgery you will have a follow up locally and restart chemotherapy about 4 weeks after your operation.
Should I continue to have cervical smears?
Normally you will have had your cervix (neck of womb) removed, so smear tests will not be necessary however please check with your consultant or gynaecology clinical nurse specialist.
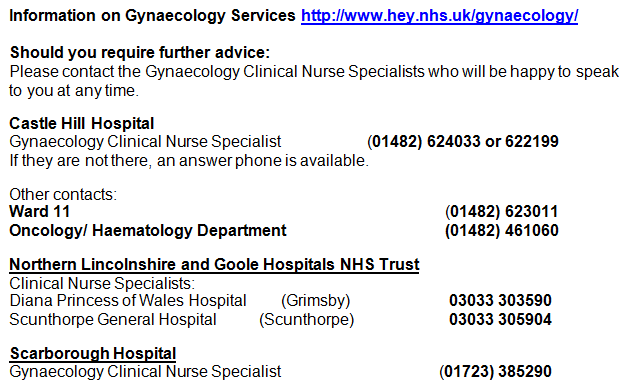
Useful contacts:
Should you require further advice: Please contact the Gynaecology Clinical Nurse Specialists who will be happy to speak to you at any time. You may find it helpful to write down any questions you may have, so that you do not forget them when you attend your appointment.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

