- Reference Number: HEY-959/2023
- Departments: Dermatology, Plastic Surgery
- Last Updated: 10 February 2023
Introduction
This leaflet has been produced to give you general information about skin and lymph node examination. Most of your questions should have been answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
Why do I need to check my skin and lymph nodes?
You have previously been diagnosed with a form of skin cancer and although the cancer has been removed there is the possibility that it may come back. Skin cancer can come back in the scar from where it was originally removed, appear elsewhere on the skin, or in the lymph nodes. Because you have been diagnosed with skin cancer you will be seen by the hospital for some years and although you will have your skin and lymph nodes checked at every clinic visit, we strongly advise that you self examine yourself every month.
How do I check my skin?
A new scar is lumpy to start off with and red in colour but will usually fade to a white line over time. We suggest you check your scar from where the original skin cancer was removed. Place your fingers over the scar and run them firmly across the length of the scar to feel for a lump. Look to see if the pigmentation has changed. Familiarise yourself with how your skin generally looks and feels. If you do notice any new lumps or discolouration please contact the hospital.
If you have had a malignant melanoma excised we also suggest that you frequently look at your moles. Any new moles, or moles that have changed, need to be brought to the attention of the hospital. If you notice any of the following changes in an existing mole please contact us:
- Change in size
- Irregular shape
- Irregular colour
- Inflammation
- Itching or change in sensation
- Crusting or bleeding
How do I check my Lymph nodes?
Lymph nodes are part of the lymphatic system. The lymphatic system is made up of vessels (similar to blood vessels) that drain away excess fluid from the body. Fluid drains from these vessels into the lymph nodes. A large collection of these lymph nodes can be found in your armpits, groins and the neck area. The doctors may also refer to the lymph nodes as glands. Skin cancer when it spreads can travel down the lymph vessels and lodge in the lymph nodes. When the cancer has reached a significant size in the lymph node it can be felt by examining the area.
To examine your lymph nodes ensure you are comfortable and relaxed before you begin. With your fingertips gently move them over the neck, armpit and groin area in a circular motion. Use your right hand to examine the right side of your body, except for the armpit area and vice versa.
If you feel a node, do not panic, as it could be due to infection or inflammation. If it is still present after a week, please contact the hospital.
Sun protection advice
The most common cause of skin cancer is sun exposure. There are a number of precautions that you can take to protect skin. We advise you to:-
- Wear clothes of cotton material or natural fibres that have a closer weave and offer better protection against the sun.
- Wear a wide brimmed hat to protect the face and always wear sunglasses in strong sunlight.
- Use sun protection such as factor 30SPF sunscreen with 4 or 5 stars UVA protection. Re-apply every 2 hours and more frequently after swimming. Also pay extra attention to ears, lips and bald patches as they can burn.
- Never allow your skin to burn.
- Stay out of the sun at the hottest part of the day, usually between 11am-3pm.
- Avoid the use of sunbeds, as the radiation may contribute to the development of skin cancer.
- Avoid staying out in the sun for long periods.
Advice for melanoma patients
We know sun exposure is generally important to health because it allows your body to make vitamin D, which is crucial for bone health. There is now some evidence that vitamin D may also be especially important after the diagnosis of melanoma. Avoiding all sunlight exposure if you suffer from light sensitivity, or to reduce the risk of melanoma and other skin cancers, may be associated with vitamin D deficiency. This is very new information and we need the results from further studies before we can be sure it is right but as vitamin D is necessary for many other aspects of your health, there is no doubt that vitamin D levels are important.
Keep your vitamin D levels up.
- Eat foods that are naturally rich in vitamin D (such as oily fish and eggs) or that have been fortified with vitamin D (such as some yoghurts and cereals).
We recommend that you make an appointment with your GP so that he can assess for vitamin D levels with a blood test to see if you would benefit from vitamin D supplements.
Other sources of information:
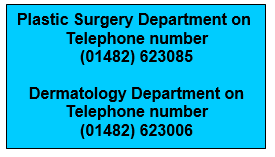
How to contact us:
If you find a lump in your scar or lymph nodes or a change in your skin please do not hesitate to contact us.
This leaflet was produced by the Plastic Surgery and Dermatology Departments, Hull University Teaching Hospitals NHS Trust and will be reviewed in February 2026.
Ref: HEY959/2023
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

