- Reference Number: HEY1125-2023
- Departments: Pain Medicine
- Last Updated: 29 September 2023
Introduction
This leaflet has been produced to give you general information about your treatment. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is sedation?
Sedation involves using small amounts of anaesthetic drugs to produce a ‘sleep-like’ state. It makes you physically and mentally relaxed, but not unconscious.
When would sedation be given?
This will be a joint decision between you and your consultant and is usually offered to reduce anxiety.
Will I remember the procedure?
Most people will remember the procedure due to the low levels of sedation used.
How will the sedation be given?
Your pain doctor will need to give you medicines(s) into a vein. They will do this through a small plastic tube placed in the vein. This is called a cannula. A needle is used to put the cannula into a vein on the back of your hand or in your arm. The anaesthetist will use a tourniquet (tight band) around the arm to make the vein more obvious.
Will the sedation cause side effects?
Sedation can cause side effects which are generally short-lived (last a few hours). This includes tiredness, dizziness, poor sleep patterns, temporary memory loss, rarely shivering, allergy, and nausea or even vomiting. Sometimes bruising may occur around the injection sites. This may be caused by a vein leaking blood around the cannula. It normally settles without treatment other than removing the cannula.
What will happen after the injections?
After the injection you will be taken to a recovery or ward area where nursing staff will observe you. You may feel a little drowsy and wish to sleep. Sometimes you will be asked to lay flat for about 30 minutes or longer. You will be assisted to sit up and your blood pressure and pulse will be checked. You will be advised when to get dressed and be given assistance to help to ensure that you can stand safely after the procedure.
Points to remember
- You may feel weak or tired for a little while after the injection so we advise that arrange for someone to stay with you for 24 hours and gently mobilise.
- You should not drive, nor operate machinery, sign legal documents, provide childcare unsupervised or drink alcohol for 24 hours.
Additional information
If you are very concerned about how you feel after the procedure, please contact either the Pain Service during office hours;-.
Pain Service Outpatient Department East Riding Community Hospital, Beverley (01482) 478868/624179
In the event of an emergency and outside normal working hours of the Pain Service (9.00am–4.00pm, Monday-Friday) please contact your local doctor Local Walk in Clinic/Minor Injuries Unit
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
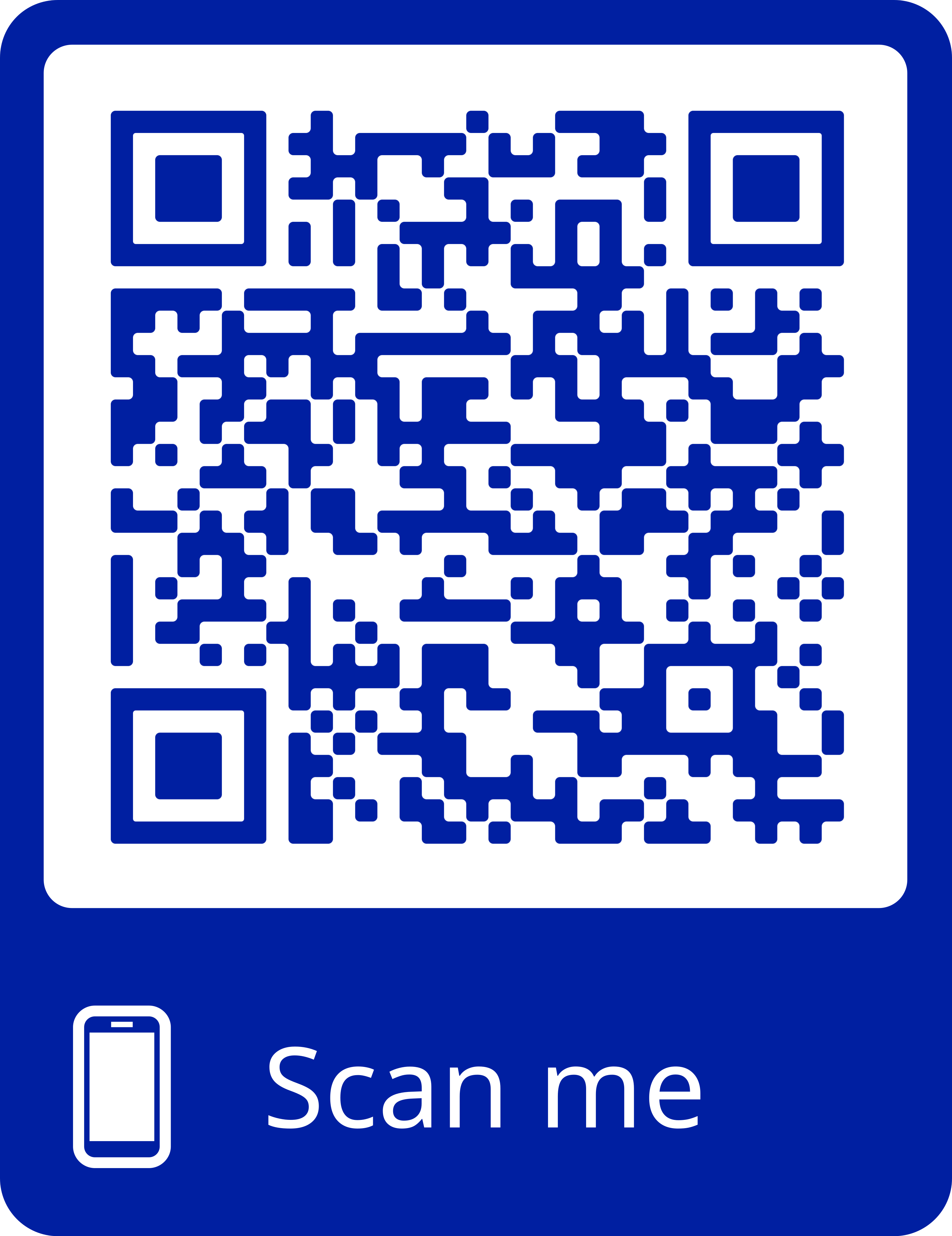
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.