- Reference Number: HEY1263/2021
- Departments: Hull Pulmonary Hypertension Service
- Last Updated: 30 November 2021
Introduction
This leaflet has been produced to give you information about right heart catheterisation, a procedure requested by your doctor to look at the different pressures in your heart. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a right heart catheter?
Your doctor has asked you to have an investigation called right heart catheterisation (RHC). RHC is a safe procedure that is normally performed during a half-day admission. RHC provides important information about the pressures in the different chambers of the heart and blood flow through the heart and pulmonary artery.
When is it used?
RHC allows the healthcare team to obtain a precise measurement of the blood pressure in the heart and pulmonary artery. RHC provides information that will confirm the diagnosis of pulmonary arterial hypertension (PAH) and confirm or exclude some other causes of pulmonary hypertension (PH).
How is it done?
If you require RHC, you will be asked to attend the Cardiology department at Castle Hill hospital as an outpatient for a pre-assessment where a nurse will perform some tests and explain the procedure.
Please let us know if you are taking any blood thinning medications such as warfarin, rivaroxaban, apixaban, dabigatran, edoxaban, heparin, dalteparin as they may need to be stopped prior to the procedure or an alternative agent may be required.
Consent
The procedure will be explained at the pre-assessment visit including the risks and benefits. You will be required to provide your written consent. The consultant performing the RHC will also go through the procedure with you in detail again on the day. The major risks (heart attack, stroke or death) are rare (between 1 in 1000 to 1 to 2000)
On the day of admission:
- The nurses will admit you to the day ward and place an identification band on you. They will take your blood pressure, heart rate and oxygen levels.
- You do not need to stop any of your regular medications (other than any anticoagulant) and you should eat and drink as normal on the day of your procedure.
- A doctor will come and discuss the procedure with you and answer any questions you may have. They will then ask you to sign a consent form for the procedure.
- You will be asked to change into a hospital gown and lie down on the trolley before you are wheeled through to a special room for the procedure.
- You will be connected to an ECG monitor and an oximeter (which measures oxygen levels in your blood). Your blood pressure will be monitored closely.
- You will be given local anaesthetic usually under the left collar bone but sometimes on the right side of your neck or at the top of your leg (depending on insertion site) which will sting for a few seconds only. The area will go numb.
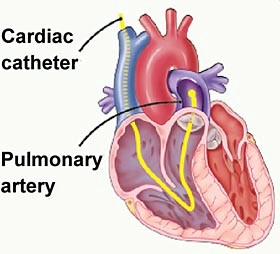
- With you lying still, a thin flexible tube called a catheter is inserted through a vein and slowly fed into your right atrium, right ventricle and then your pulmonary artery.
- The catheter is a tube about 1 metre long and as thin as spaghetti. It allows the doctor to measure the blood pressure in several places at once. This is often done with the help of X-ray pictures, which are viewed on a television monitor.
- Several blood samples are often taken using the catheter to give specific measurements of the oxygen levels in various parts of your circulation. An estimate of cardiac output (the rate of blood flow through the heart and body) is also recorded.
- Once the procedure is completed the catheter and small sheath are removed and light pressure with a piece of gauze is applied to the site where the sheath was inserted.
- The results will be available that day and the doctor will either speak to you or at a later time.
- You will be wheeled to the recovery area where you blood pressure (arm) will be monitored.
- You will normally be discharged within 1 or 2 hours.
You should NOT drive any vehicle for 24 hours after your RHC.
Contact information and hours of Pulmonary Hypertension Service
For further advice or information regarding the right heart catheter, please contact the Hull Pulmonary Hypertension Team on (01482) 622422 (24 hour answer machine) or one of the contacts below.
Specialist Nurses:
Mark Major 07769 742092
Amanda Bell 07585 998695
Secretarial support:
Nicky McKenzie (01482) 624067
Sarah Constable (01482) 622422
The Hull Pulmonary Hypertension Service operates Monday to Friday 9.00am to 5.00pm.
For urgent issues outside these hours please contact your doctor or NHS111.
NHS Choices
NHS Choices provides online information and guidance on all aspects of health and healthcare, to help you make decisions about your health. Web: www.nhs.uk
NHS 111
You can contact NHS 111 when you need medical help fast but not a 999 emergency. NHS 111 is available 24 hours a day, 365 days a year. Calls are free from landlines and mobile phones.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.
