- Reference Number: HEY-935/2017
- Departments: Speech and Language
- Last Updated: 1 September 2017
Introduction
This leaflet has been produced to give you and your family general information about some of the eating and drinking difficulties you may experience as a result of having respiratory difficulties. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the Speech and Language Therapist, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
What is dysphagia?
- Dysphagia means ‘a swallowing difficulty’.
- As many of the muscles involved in swallowing and br
 eathing have dual roles (Shaker et al1992), problems in one may lead to a difficulty in the other.
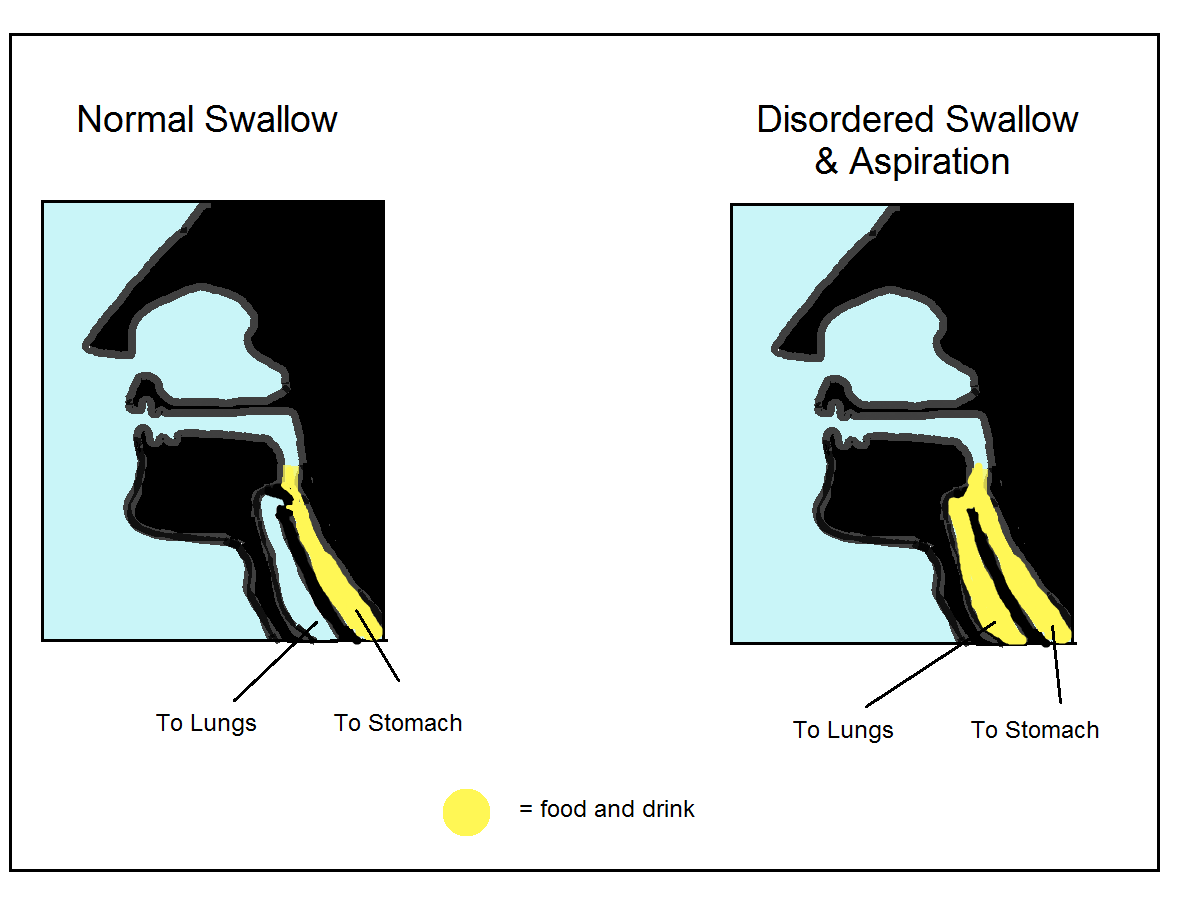
eathing have dual roles (Shaker et al1992), problems in one may lead to a difficulty in the other. - There are risks associated with having dysphagia including, aspiration (food going down into your lungs), choking, poor nutrition and reduced quality of life.
- It is common for individuals with breathing difficulties to have problems eating and drinking. 27% of people who suffer from COPD (Chronic Obstructive Pulmonary Disease) have a dysphagia. (McKinstry et al 2009).
How is swallowing linked to breathing?
For this process to occur well, the body must also co-ordinate the breathing cycle with the swallow. The swallow temporarily interrupts breathing. The moment you swallow, you must momentarily hold your breath to close the airway (this prevents any food or fluid from entering the lungs). The usual cycle is:Swallowing is a highly complex process involving the coordination of more than 26 muscles and 6 nerves. We swallow around 600 times a day and the normal pattern of swallowing happens quickly and should only take a few seconds to complete.
Breathe out –> hold breath to protect airway approximately 1 – 1.5 seconds (apnoeic episode) –> swallow –> continue to breath out a little –> breathe in –> repeat.
People who have a breathing difficulty may breathe in after swallowing rather than breathe out. This can increase the risk of food and drink being inhaled into the open airway (Shaker et al 1992). Additionally, if you have difficulties triggering a strong cough, this may reduce your ability to sufficiently protect your airway if something went down the wrong way.
How could this affect you?
- Muscles feel tired and weak.
- An increased rate of breathing during eating and drinking can increase the likelihood of food and drink going down the wrong way. This may also cause a chest infection.
- If you have a breathing problem, you may require oxygen therapy and wear an oxygen mask. This may make eating and drinking more difficult.
- Dry mouth (xerostomia) is common if you wear an oxygen mask or you mouth breathe. Chewing and clearing food from your mouth can be difficult when you suffer from xerostomia.
- Breathing difficulties have been linked to the increased likelihood of bringing food and drink back up from the stomach (this is called reflux but is commonly known as indigestion). Sometimes this can come up from the stomach and enter into the airway from the food pipe; you may feel bloated or experience belching. It may also cause irritation in the airway or cause you to cough.
- An increased work of breathing uses up more energy and muscles can tire quickly. If you are exhausted or feel weak you may find that it takes longer to complete your meals and you may eat and drink less. This may mean you miss out on important nutrients and/or lose weight.
Signs that you may have respiratory dysphagia
- Increased shortness of breath during mealtimes.
- Reduced appetite.
- Difficulty chewing and avoiding difficult textures e.g. chewy/crunchy foods.
- Wet or gurgly voice during and/or after swallowing.
- Taking much longer to complete a meal.
- Sensation of food sticking in the throat.
- Increased work of breathing.
- Getting tired during and after eating and drinking.
- Anxious when eating or drinking.
- Experiencing a sensation of feeling ‘full-up’ even though you have only eaten very small amounts.
- Experiencing more acid indigestion (reflux).
- Coughing during or just after eating and drinking.
- Chestiness or recurrent chest infections.
- Difficulties taking tablets.
Advice on how you can help:
Before eating and drinking
- If you can have your oxygen via nasal cannula this would be preferable whilst you are eating and drinking. If you use a face mask, it may be helpful for someone to assist you at mealtimes.
- Making sure that your mouth is clean and moist by regularly brushing your teeth and gums (or clean your dentures) to reduce bacteria build up in your mouth – speak to your nurse/GP if you need saliva replacement products.
- It is very important that you sit fully upright, if you need assistance achieving this please ask someone to help you.
- If you have secretions stuck in your throat/back of mouth, try to cough to clear these first. Speak to a nurse if you require assistance clearing your secretions.
- If you wear dentures make sure these fit well and are comfortable, if they are loose or ill-fitting they may cause more of a problem.
- Ensure you have easy access to all your cutlery and food.
- It would be helpful to have a relaxed and comfortable environment during mealtimes – turn off any distracting music/tv etc and avoid talking whilst eating and drinking. Try to relax your whole body as much as possible.
- Make sure you are well rested before eating and drinking. Be aware that food preparation may be tiring.
- If you are extremely breathless please seek advice from a medical professional as eating and drinking may become very difficult.
During and after eating and drinking
- Do not use spouts or straws unless they have been specifically recommended.
- Eat slowly and take smaller mouthfuls. It may help to take softer foods which require less chewing.
- If your mouth is feeling dry, take a sip of fluid when you need to but be aware that alternating drinks with mouthfuls of food may be difficult.
- You may benefit from doing an extra swallow to clear any food residue.
- Avoid continuous drinking; ensure you take one sip at a time.
- Attempt to breathe out immediately after a swallow.
- You may find eating little and often easier. Select high calorie options if you are struggling to eat enough.
- If you are concerned about your nutrition you can ask the nurse or dietitian about what extra snacks are available.
- Remain upright for at least 30 minutes after a meal.
If you experience reflux or heartburn, discuss anti-reflux medication with your doctor or GP. If you have been prescribed reflux medications ensure you are taking these correctly.
If you are concerned about a family members swallowing, please contact their GP. Should you require further eating, drinking or swallowing advice, please do not hesitate to contact the Speech & Language Therapy Department telephone no: (01482) 604331.
Credit is to be given to Leeds Community Healthcare NHS Trust for the supply of additional content to produce this leaflet. This final copy was produced by the Speech and Language Therapy Department, Hull University Teaching Hospitals NHS Trust with the help of a Speech and Language Therapist in Northumberland, Tyne and Wear.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

