- Reference Number: HEY-071/2020
- Departments: Radiotherapy
- Last Updated: 7 December 2020
Introduction
This leaflet has been produced to give you general information about radiotherapy to the prostate. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
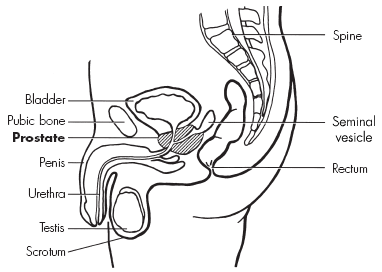
Where is the prostate?
The prostate is a walnut sized gland found only in men that lies just below the base of the bladder and in front of the rectum.
Image Copyright: Macmillan Cancer Support
What is radiotherapy?
Radiotherapy, also known as radiation treatment, is the controlled use of high energy X-rays to treat many different types of cancer. The X-rays are produced electronically by a machine called a Linear Accelerator (Linac) and takes 10 – 15 minutes.
Radiotherapy works by causing chemical and physical damage to the cancer cells in the treatment area. Although some normal healthy cells are also affected these are able to recover and repair themselves.
Radiotherapy has a number of different benefits from curing some cancers after surgery but also may be used as symptom control. Radiotherapy does not make you radioactive and you are safe to be around people including children whilst you are on treatment.
Your clinical oncology consultant will have already discussed the treatment, side effects and gained consent for you to receive your radiotherapy. There are several stages prior to you actually commencing your treatment.
Planning your treatment
Your first appointment in the Radiotherapy Department will be a planning appointment. This appointment will be approximately 30 – 60 minutes in duration.
A member of the Radiotherapy Team will talk to you before any procedure is carried out to obtain your consent for this process. They will also discuss possible side effects of treatment and how they can be managed. A specialist X-ray machine called a CT (Computed Tomography) scanner will be used as part of the planning process. This machine takes images in slices whilst you lie on a couch that moves backwards and forwards through the hole of the machine, as shown in the next picture.
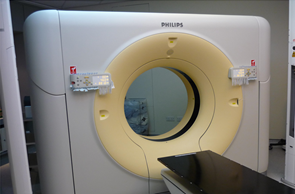
Image from Radiotherapy Department
In the CT room you are helped into the correct position on the couch and we will have to loosen/remove your clothing in the area of your pelvis. Some temporary skin marks will be drawn onto your pelvic area. The staff will then leave the room to perform the scan. The staff will then use a sterile needle and ink to replace the temporary marks to permanent marks. These marks will only be the size of a freckle and allow the radiotherapy staff to accurately align and reproduce the correct position daily for treatment.
You may have already had a CT scan for diagnostic purposes, however the information obtained from this scan is used to produce your individual treatment plan. The CT staff will confirm your treatment start date before you leave the department.
Radiotherapy treatment – what happens on the first day?
On your first day and each day afterwards, when you attend please book in at the radiotherapy reception desk. You will be asked to take a seat either in the main waiting area or directed to a specific waiting area. A radiographer will come and collect you from the waiting area and advise you to start drinking on your first day. The radiographers will not inform you to do this daily so please follow these instructions:
- Arrive 45 minutes before your appointment time to allow enough time to drink and process the water required
- Empty your bladder upon arrival to the department
- Drink the amount of water specified by the Radiographers on day one (usually 4 cups / 800ml). This should be done over a 15 minute period unless you have been informed otherwise
- It is important to remember that it takes approximately 30 minutes for the liquid to reach your bladder; therefore your final cup of water should be 30 minutes BEFORE your appointment time.
- Any delays will be displayed on the screens in the waiting area; this should be taken into consideration when filling your bladder. For example, if there is a 30 minute delay start drinking your water 30 minutes later than you originally would have. Each patient’s appointment should take approximately 15 minutes so this can be used as an indication of when you will be taken through for your treatment. However please be aware that the patient queue is subject to change due to multiple factors.
- If you ever feel unable to hold your bladder or have any other questions, please speak to a radiographer.
What happens during treatment?
Radiotherapy is painless and usually takes 10 – 15 minutes to deliver. . There are two types of Linear Accelerator (Linac) machines in this department, they may look different but they deliver the same treatment.
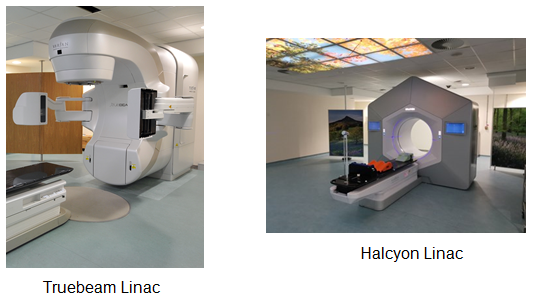
Image from Radiotherapy Department
Your bladder will need to be full and your bowels need to be empty prior to your treatment each day. If you have been prescribed products (i.e. rectal suppositories) by your consultant please continue to take as advised. Both of these are very important for the accuracy of your treatment.
A member of staff will escort you into the treatment room. A curtained private changing area is available should items of clothing need to be removed, maintaining your privacy at all times.
The radiographers will then assist you into the correct treatment position on the couch, as you were for your planning appointment. The radiographers are controlling the Linac machine at all times and may seem close but will not touch you. Once you are set up in the correct position the staff will then leave the room for a few minutes to commence treatment.
The machine is being controlled by the staff outside in the control area which will rotate around you in different directions. These rotations cannot be seen on the Halcyon machine due to the cover around the machine. The radiographers are watching you at all times on the TV monitors, should you need to attract their attention if any assistance is required. You will not feel or see anything during your treatment however you will hear a buzzing sound when the treatment is being delivered.
Reviews during your treatment
You will have regular weekly reviews with a radiographer as you progress through your treatment to assess how you are coping with any side effects. You may be referred to one of our nursing team if further medical advice or intervention is required.
Side effects of your treatment
Side effects and reactions from the treatment may be experienced as you progress through your treatment. Every individual is different. You may experience some side effects and at varying levels – these are normal and temporary. You can speak to your radiotherapy team regarding how you can control the side effects, or if your symptoms worsen we can advise and treat you.
Listed below are some of the most common side effects experienced. These usually begin approximately 2 – 3 weeks into treatment and may last for several weeks. They will continue for a short while once you have completed your radiotherapy but will slowly settle down after that.
Urinary problems
You may experience changes to your urinary symptoms. These include:
- Burning or stinging sensation when you pass urine, also known as cystitis.
- Passing urine more frequently, especially during the night (nocturia).
- An increased urgency to pass urine but unable to do so.
Following the steps below may help with the above symptoms:
- Ensure that you are drinking enough fluid and increase if necessary. We recommend that you 2 litres of water a day.
- Try to limit/avoid smoking, drinking alcohol and caffeinated drinks (i.e. tea, coffee, soft drinks) because they can make urinary problems worse as they can irritate the bladder.
- Drinking a daily glass of cranberry juice may help prevent urinary infections, though you should NOT do this if you are taking warfarin.
Bowel problems
Changes in your bowel habits/motions may occur as radiotherapy may irritate the bowel. These can include:
- Loose motions/diarrhoea. This can easily be treated with medication.
- The urge to want to open your bowels more frequently but without passing anything (tenesmus) or only a small stool.
We do not recommend you alter your diet drastically in any way but if you do begin to experience any of the above symptoms speak to a radiographer or nurse who will be able to advise you.
Skin reactions
Sometimes radiotherapy may cause skin in the treated area to become sore or pink, around the groin area and in between the buttocks. This is rare and advice will be given on how to care for your skin if this does happen.
Fatigue / tiredness
Some patients may experience feeling tired more than usual during treatment. This could be due to having to get up several times during the night or travelling a long way for daily treatment. Try to rest when you feel the need. Normal energy levels will return approximately one month after your treatment has finished.
Late side effects
With the use of modern planning techniques the aim is to reduce the chance of late side effects from happening that may occur some months or even years after completion of treatment.
Bladder
- Incontinence (unable to hold as much urine as previously).
- Urinary frequency.
- Thinning of the lining of the bladder.
Bowels
- Diarrhoea or more frequent bowel movements (common).
- Narrowing of the bowel.
- Bleeding from the rectum (contact your clinical oncologist).
- Inflammation of the lining of the rectum (proctitis). Please contact your clinical oncologist if you need to discuss this.
Impotence (difficulties in getting an erection)
This may be due to radiotherapy, hormone treatment or surgery and occurs in 25% of men. If this problem continues please consult your doctor.
Infertility
Most treatments for cancer cause infertility, meaning you will no longer be able to father a child. You may wish to discuss this further with your consultant prior to radiotherapy.
What happens at the end of your treatment?
Once you have completed your course of radiotherapy treatment you will receive a follow up appointment either on your last day, or your appointment will be sent to you in the post, to return to see your consultant oncologist at the hospital where you were first seen. This is usually about 4 – 6 weeks after treatment has finished, as it is necessary to allow any side effects experienced to settle down. Your consultant will then decide if any further tests or appointments are necessary.
Hormone therapy
Hormone therapy may be given in addition to radiotherapy – this is known as adjuvant therapy. Hormones control the growth and activity of normal cells and are naturally produced in the body.
Your doctor may advise that you could benefit from hormone treatment. Prostate cancer depends on the hormone “testosterone” which is produced by the testicles, stimulated by a hormone called a leutenising hormone, produced by the pituitary gland.
Hormonal therapies stop the production of leutenising hormone produced by the pituitary gland thereby reducing the production of testosterone in men.
How is hormone therapy given?
Hormone therapy is usually given by injection under the skin of the abdomen (subcutaneously). It is given as an injection every four weeks (monthly), or as a longer-acting preparation every 12 weeks. The injections are usually given by your doctor or nurse at your surgery.
What are the side effects of hormone therapy?
The most common side effects from hormone therapy are outlined below, some men may experience more than others. If you have any concerns please speak to your doctor.
Hot flushes and sweating
Ways to help reduce these include:
- Reducing the amount of caffeinated drinks (i.e. tea and coffee on a daily basis).
- Reducing alcohol and nicotine.
Weight gain and tiredness
You may notice that you gain weight and feel less energetic than usual. This usually improves when hormonal treatment stops.
Sexual dysfunction
Loss of sex drive (libido) and erection difficulties (impotence) can occur.
Breast tenderness or fullness
You may sometimes notice slight breast swelling and tenderness known as gynaecomastia.
Skin rashes
Some people experience skin rashes.
Sore joints
Some people may have soreness in their joints, but this is usually mild and will stop when the treatment is finished.
Bone thinning (osteoporosis)
You may be at more risk of this if you are taking hormone therapy for longer periods of time. Your doctor can give you advice on how it can be monitored and treated, if needed. Let your doctor know if you have any discomfort in your bones or joints.
How long will I be on hormone therapy for?
Your doctor will discuss the length of treatment that they feel is appropriate for your situation. It is often given for several months or even years.
Once your hormone therapy is completed any side effects should stop or disappear.
Advice and support services
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you.
Radiographers
Therapy radiographers are specialist healthcare professionals who are trained to plan and deliver radiotherapy treatment and to use the specialised equipment. You will usually see the same team of radiographers on a daily basis and they can help you with any questions or problems, or refer you to another member of the team as necessary.
Radiotherapy Nursing Team
The team consists of registered nurses and clinical support workers (CSWs) based within the Radiotherapy Department. They actively support and advise patients receiving radiotherapy treatment. They are able to make appropriate referrals and offer advice to patients and their families/carers.
Health Centre
The primary aim of our Health Centre is to help patients and their families to have the best possible health and quality of life during and after treatment. Open to all oncology patients and their families in offering an informal atmosphere to those who wish to “drop in” to the centre. Specially trained staff are able to advise you on different aspects of coping with cancer. For further information about the Health Centre ask at the main reception for the leaflet entitled “The Oncology Health Centre”.
The Health Centre is located in the main reception of the Queen’s Centre for Oncology and Haematology at Castle Hill Hospital. Opening times are Monday – Friday 9.00am to 5.00pm.
Macmillan Sexuality Counsellor
For queries or to arrange an appointment please contact:
Oncology Health Centre,
Queen’s Centre,
Castle Hill Hospital,
Telephone: (01482) 461232 / 461060.
Below are contact details of useful organisations that provide information about cancer including radiotherapy treatments:
Macmillan Cancer Support
Provides information from specialist nurses on all aspects of cancer and its treatment and on the practical and emotional aspects of living with cancer.
You can drop into the Macmillan Cancer Information Centre at the Queens Centre or call them on (01482) 461154 (Monday – Friday 9.00am to 5.00pm
Alternatively free-phone national help line 0808 808 000 (Monday – Friday 9.00am – 8.00pm
On line: http://www.macmillan.org.uk
Write to: Macmillan Cancer Support, 89 Albert Embankment, London, SE1 7UQ
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Information and Support Team on telephone number (01482) 461206.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.