- Reference Number: HEY-219/2022
- Departments: Endoscopy
- Last Updated: 10 November 2022
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should have been answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team who has been caring for you.
Endoscopy Department contact numbers: Hull Royal Infirmary (01482) 674790 (direct line) Castle Hill Hospital (01482) 622069 (direct line)
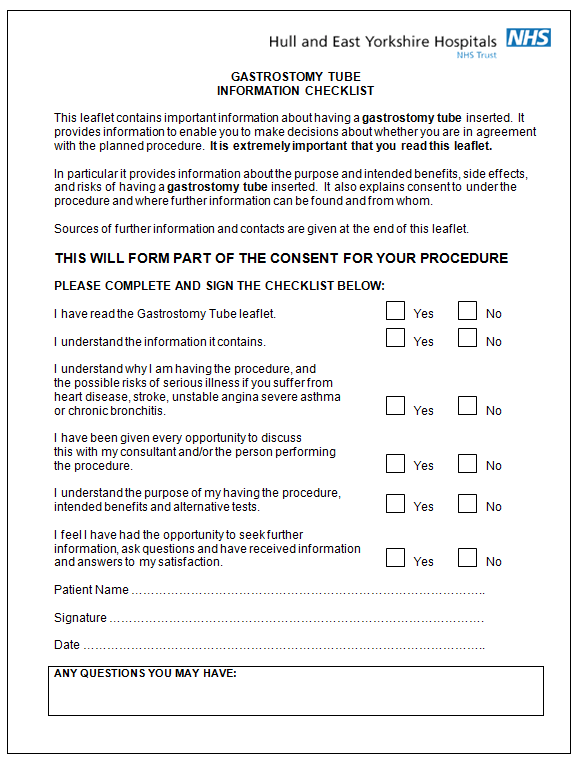
PLEASE DETACH THE INFORMATION CHECKLIST AND BRING IT WITH YOU
What is a Percutaneous Endoscopic Gastrostomy (PEG)?
You have probably been troubled by some symptoms, which have led to your doctor advising that you will now benefit from nutritional support (help with taking food and drink into your body). You may be finding food especially solid food, e.g. meat and bread, very difficult to swallow, if not impossible and may be even liquids or you may be having an operation or treatment that could affect your swallowing.
The method of support your doctor believes is best for you is a gastrostomy tube, you may hear this called a PEG (Percutaneous Endoscopic Gastrostomy) tube. PEG is the technique for putting the gastrostomy tube in place. Percutaneous means ‘through the skin’. An endoscope is the long flexible tube passed through the mouth and into the stomach.
A member of the PEG team will contact you to discuss the procedure with you.
What does this involve?
It will mean you having a test, which allows the endoscopists to look directly at the lining of the stomach/gullet (known as an upper GI endoscopy). You will be given a sedative and the doctor will pass a slim flexible tube with a light on (endoscope) through your mouth and into your gullet (oesophagus) until it reaches your stomach. The endoscopist will also look at the first part of your small bowel.
After numbing your skin with a local anaesthetic, a small cut is made on the upper part of your abdomen. The gastrostomy tube is placed through this cut.
The tube will not fall out because there is a bumper at the end of the tube inside the stomach. There is also a small plastic fixator on the outside of your abdomen, which lies close to the skin. This keeps the tube from sliding in and out of the opening. At the end of your tube there is a feeding adaptor. This connects to a syringe or feeding set. The adaptor closes at the end when the tube is not in use.
The PEG procedure will take about 20 minutes.
What if I refuse to have a gastrostomy tube?
This will not alter the manner in which we treat you and your standard of care will not change. You will need to discuss this and alternatives to this means of nutritional support with your doctor/specialist team.
Who will do the procedures?
An endoscopist who is specially trained and experienced in performing the procedure will carry out the Percutaneous Endoscopic Gastrostomy. A senior nurse or doctor who is specially trained and experienced will insert the gastrostomy tube.
Can there be any complications or risks?
Sedation
Some people, for reasons we still do not fully understand, are particularly sensitive to this drug. The breathing can be too shallow and too slow. In these cases we stop the examination, give more oxygen and if required we can give an antidote, which reverses the effect of the sedation. This is usually all that is needed and the person recovers with no ill or lasting effects.
In some cases, when people have another serious illness e.g., heart disease, stroke, unstable angina, severe asthma or chronic bronchitis, the sedation drug can cause difficulty in breathing. Severe reactions are rare however a drop in oxygen levels occurs in 70 patients out of 100 and is why we monitor breathing and heartbeat throughout; and why we give oxygen by nasal tubes.
Infection
The point at which the gastrostomy tube enters the body is known as the stoma site. There is a risk that this opening may become infected. In order to reduce this risk you will be given antibiotics into the vein before the procedure. While you are on the ward your nurse will check the stoma at regular intervals. If you do get an infection the stoma may become hot, itchy and painful. You must tell the nurses if this happens to you, as you may need treatment.
Aspiration Pneumonia
If stomach juices enter the lungs they can cause pneumonia. To reduce this risk, you are asked not to eat and drink 6 hours before the procedure. In addition a nurse will stay with you during the procedure and whilst you are sedated.
Haemorrhage
Insertion of a gastrostomy tube carries a risk of haemorrhage (bleeding) but it is still rare. As with all endoscopies, there is a small risk of perforation (making a hole) of the gut. If this happens, sometimes an operation is needed.
Where will the procedure be performed?
The placement of your gastrostomy tube is performed in the Endoscopy Department. Specially trained doctors and nurses work in the department and are very experienced in performing endoscopy, inserting gastrostomy tubes and the care they involve. All the staff will help to make your stay as easy and dignified as possible. Please do not be afraid to ask questions.
It will be done at Hull Royal Infirmary or Castle Hill Hospital depending on where your consultant is based. Please make sure that you go to the correct Endoscopy Department. Directions will be given with your appointment letter.
How do I prepare for the procedure?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination. Complete the health questionnaire sent/given to you as fully as possible.
To allow for a clear view, your stomach and first part of your intestine needs to be empty.
You should not have any thing to eat and drink for at least 6 hours before your test. Do take any regular medicines up to this point.
If you have diabetes (especially taking insulin) or you have serious heart, lung or kidney problems, or concerned that a health problem you have may be affected, then contact the Endoscopy Department at the hospital where you are having your examination (see contact numbers).
WARFARIN – These are blood thinning tablets and usually have to be stopped for a period of time before your test, please contact your endoscopy department for advice.
LATEX – Please inform the department if you have a confirmed latex allergy as this will affect your appointment time.
Creutzfeldt-Jakob disease/variant Creutzfeldt-Jakob disease CJD – Please inform the department if you have been notified that you are at risk of CJD/vCJD for public health reasons.
CLOPIDOGREL (PLAVIX) – Please inform the department if you are taking these tablets as these usually need to be stopped prior to your procedure.
PREGNANCY – It is important that you inform us if there is a possibility that you may be pregnant. Any information you share with us will be kept strictly confidential.
If you take any of the following blood thinning tablets please contact the Endoscopy Department before your appointment for further advice: APIXABAN, RIVAROXABAN, DABIGATRAN, ARGATROBAN OR EDOXABAN
In most cases you will be admitted to a ward before your procedure if you are not already an inpatient.
Do I need sedation?
Yes. People have sedation to keep them comfortable while the endoscopist carries out the procedure. Sedation is given through a flexible needle in the back of your hand or arm. It makes you feel light headed and relaxed but does not put you to sleep. You can still respond to what is happening.
Do I really need someone with me after sedation?
Yes, this is very important. The sedation given can have effects, which last some 24 hours after the test. You can become forgetful and also sleepy again. Your test may be cancelled if you do not arrange to have someone to collect you and stay with you for the next 24 hours.
We strongly recommend that for the next 24 hours you:
- Do not drive
- Do not return to work or operate machinery
- Do not sign any important/or legal documents
- Are not left alone, you may be at risk of injuring yourself
- Are not left alone to care for children
If you are an outpatient, the person accompanying you will be contacted to collect you. If you are an inpatient you will be transferred back to your ward.
What happens to me in the Endoscopy Department?
On the day of your procedure you will be transferred from the ward to the Endoscopy Department. Your named nurse who will stay with you throughout your procedure will meet you. The nurse will explain the procedure to you again and ask any questions or concerns you may have. At this time we will check your blood pressure, pulse and oxygen levels and ask you a few questions about your general health (this may have been done on the ward before you arrive). Please feel free to ask questions.
We will ask you questions about your general health and work through the health questionnaire you have completed for us. If you wear glasses or dentures, you will be asked to remove them. The endoscopist will meet you and explain the test to you.
You will both sign a consent form unless you have already done this. It is to show you understand what will happen and agree to the procedure being performed. At any point during the procedure you can withdraw your consent and ask for the procedure to stop. If this happens the endoscopist will stop the test and take the scope out. If you have any queries or worries, please tell us.
You will be taken to the examination room and made comfortable on your back on a bed. To keep your mouth open, a plastic mouth guard will be placed between your teeth. A fine plastic tube will rest by your nostrils to give you some oxygen. A probe will be placed on your finger to monitor your oxygen levels and pulse rate. If you are having sedation it will be given now and you will feel relaxed and light headed.
What will the test feel like?
You may feel the tube gently slide over your tongue and down your gullet. It will not be painful, or interfere with your breathing but it can be uncomfortable. If you get a lot of saliva, the nurse will clear it with a thin plastic tube. You may feel the tube move around in your stomach. Some air will be passed down the tube to inflate your stomach to allow a clear view. The nurse will then prod your tummy to find a suitable place for the PEG to go. A small cut will be made and the PEG will be pulled through that hole. This can be uncomfortable. The test normally takes 20 minutes or less.
What happens when the procedure is finished?
You will need to rest on a trolley in the recovery room for approximately 30 minutes. We will check your blood pressure, pulse and oxygen levels on a regular basis. You will need to stay in the department after this procedure so we can monitor you closely. Once you have recovered from your sedation you will be transferred back to your ward. The staff will be given specific instructions on when feeding can commence though the tube and how to care for the tube.
What will it feel like afterwards?
It is quite likely that the back of your throat will feel sore for the rest of the day. You may feel bloated if some air remains in your stomach. Both discomforts usually pass without any medication. You may feel drowsy for a few hours after the procedure until the sedation has worn off completely.
The stoma (an opening through the abdomen created surgically) may feel sore once the local anaesthetic has worn off. Your nurse will be able to give you some pain relief medication to soothe this. You will feel a short tube on your abdomen; this is the gastrostomy tube. Do not worry it will not fall out and you can move about normally.
When will the tube feed commence?
The hospital dietician will devise a feeding regime for you and advise the nursing staff when to start the feed. It is usually within 12 hours of the procedure. Your feed will usually take the form of a commercially prepared liquid diet that will contain all the nutrients that you would receive from a health balanced diet. A leaflet describing your gastrostomy tube and its care will also be given to you. You will be provided a PEG passport that documents details of your gastrostomy tube. This is to go home with you after you have been discharged.
Further information
If you require further information about your test your GP, consultant, and the Endoscopy Department is a valuable source of information. Further information about your rights with regards to consent can be found in the following documents: These are free of charge.
- Department of Health (2001), Guide to Consent for Examination or Treatment
- Department of Health (2001), Consent – What you have a right to expect
- A Guide for Adults. (Available from the Endoscopy Department)
- A Guide for Relatives and Carers. (Available from the Endoscopy Department)
Visit the Department of Health’s website at: www.doh.gov.uk and, for consent: www.doh.gov.uk/consent
Useful contact numbers:
The Endoscopy Department, Castle Hill Hospital(01482) 622069 Monday – Friday: 8.00am – 5.00pm
The Endoscopy Department, Hull Royal Infirmary(01482) 674790 Monday – Friday 8.00am – 5.00pm
Ward 100 Hull Royal Infirmary Out of hours (01482) 674860
What do the words in the leaflet mean?
- Abdomen: The tummy or belly.
- Consent: This is the agreement between you and the endoscopist. You are agreeing to have investigations or treatment and that you understand the purpose, benefits, alternatives and risks. You and the endoscopist during this process usually sign a consent form.
- Endoscopy Department: The place where your procedure takes place.
- Endoscope: A tube for looking inside the body.
- Endoscopist: This can either be your consultant, an experienced and trained doctor or an experienced and specially trained practitioner.
- Jejunum: Upper half of the small bowel between duodenum and ileum. The food is absorbed here.
- Oesophagus: The gullet. The pipe leading from the mouth to the stomach.
- Percutaneous: Through the skin.
- Stoma: An opening, through the abdomen, created surgically.
This leaflet has been written with the help, support, advice and collaboration of:
- Consultants of the Department of Gastroenterology
- Consultants of the Surgical Department
- Staff of the Endoscopy Department
- Patients attending the Endoscopy Department
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

