- Reference Number: HEY-1291/2022
- Departments: Orthopaedics
- Last Updated: 1 May 2022
Introduction
This leaflet has been produced to give you general information about your injury. We understand you may not have seen a clinician face to face in fracture clinic however, most of your questions should be answered by this leaflet. If after reading it, you have any concerns or require further explanation, please do not hesitate to contact the fracture clinic team. Contact details are available at the end of this leaflet.
What is a patella dislocation?
A dislocated knee cap (patella) is a common knee injury. A blow or an awkward twist of your knee often causes it. The patella normally sits at the front of the knee, it glides within a groove in the thigh bone (femur) when you bend or straighten your leg.
When the kneecap (patella) dislocates, it comes out of the groove and the tissues around it can be torn or stretched.
How should this injury be treated?
In most cases, a brace is not required and a patella dislocation can be managed simply in a tubigrip bandage.
Initially you may benefit from using crutches. This may help you to walk in a normal pattern without limping. If you are using only one crutch, it is important you hold it in the opposite hand to your injured side.
What if I need pain relief?
To manage your pain, we advise that you regularly take simple pain relief, which can be bought over the counter. If you have allergies or conditions, which prevent the use of pain-relieving or anti-inflammatory medication, please seek advice from your doctor or a pharmacist.
What should I do in the first few days after the injury?
The most important initial treatment is aimed at controlling the pain and swelling by following the principles of RICE:
R REST
Complete rest is not advisable but it is important that you prevent putting the knee under strain in the early stages of healing.
The movements below should be practiced 10 times, three to four times every day. These exercises should not cause excessive pain and so you may find initially you cannot move your knee far but this will improve as the injury starts to heal:
- In sitting, pull your toes and ankle up towards you.
To assist this movement, place a scarf or towel around your foot and gently pull your foot up, by pulling the scarf with your hands. Hold this position for five seconds.

Now point your toes away from you and hold for five seconds.

- While lying or sitting put a scarf around your foot and gently bend and straighten your knee within the range that is comfortable for you.
The scarf will just help you control the movement

I ICE
Ice will help reduce the pain in your knee and so should be applied for 10 – 15 minutes before performing the exercises above. This will help to reduce the swelling.
There are many different ways in which ice can be applied however crushed ice, in the form of frozen peas for example, is the most effective. Whichever method you choose it is important that you wrap the ice in a damp towel, in order to prevent it from ‘burning’ the skin.
Please Note:
- Only use an ice pack on areas that have normal skin sensation i.e. where you can feel hot and cold
- Do not apply ice to an open wound
- Do not apply an ice pack to an area that has poor circulation
- When you apply ice to your skin, check the skin every five minutes and stop using it if:
- the area becomes white, blue or blotchy
- the area becomes excessively painful, numb or tingles
C COMPRESSION
You may have been given a tubigrip to wear on your knee, to help control your swelling. It is important this is removed if you develop any signs of poor circulation such as tingling, numbness, blueness of the skin of the foot and increasing pain. The tubigrip should be removed when you go to bed at night as when you are asleep you cannot monitor these symptoms.
E ELEVATION
The ankle should be elevated above the level of the heart as much as possible, as this will reduce and prevent swelling in the knee.
Carrying out the movements of the ankle described above, while the leg is elevated, may help to reduce any swelling further.

What not to do
Initially you should avoid twisting your knee and also avoid trying the activity you were doing when it dislocated. Do not allow your leg to become stiff or weak, as this will prolong your recovery.
Walking and exercise
Walking normally on the injured leg as soon as possible after the injury will allow the muscles to regain their usual strength and prevent the knee from giving way.

Normal walking means that you strike your heel to the floor first and straighten out the knee, then rock forward onto your foot and lastly push off from your toes.
If you are struggling to do this without using crutches please discuss it with your physiotherapist.
If you follow the basic advice, healing of the soft tissues around the knee normally takes around six weeks. However, everyone recovers from injuries at different rates and it is dependent on the severity of the injury and the presence of any other medical problems.
Most patients recover well from a dislocated patella however to give yourself the best chance of a good recovery it is important to work hard at the following simple exercises. These exercises will help you to regain full function, flexibility and strength and also reduce the risk of the injury reoccurring.
- Stand facing a chair and step backwards with your injured leg.

Keep this leg straight with your toes pointing forward and the heel on the floor.
Now bend your other knee until you feel a stretch in the calf of your injured leg. Hold this for 30 seconds and repeat three times per day.
2. Hold the thigh of your injured leg with both your hands so that the knee is pointing upwards.

Now straighten your knee as much as possible by lift your foot up towards the ceiling.
Hold this for 30 seconds and repeat three times per day.
3. Lay on your stomach on a bed or on the floor. Bend your injured knee as far as you feel comfortable

Now wrap the uninjured leg over the injured side and gently try to bend it a little further. Do not force.
Hold this for 30 seconds and repeat three times per day.
4. This exercise was mentioned earlier but is really important to continue with in order in regain full movement in the knee

While in this seated position, wrap a long scarf around your foot and start gently bending your knee, using your arms to help assist you. Hold the knee and most bent position you can for 10 seconds.
Now straight the knee fully and repeat ten times.
5. Stay in the same position as exercise 4. This time use your thigh muscles to push the knee straight.
This can often be difficult to do following this type of injury. As you try to push your knee down your heel should raise off the bed slightly.
Hold 5 seconds, repeat 10 times.
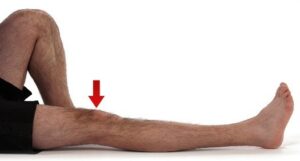
6. Lie down on your back with a rolled towel under your thigh, just above the knee.

Lift your heel up off the floor or bed and straight your knee as much as you can, without lifting the leg from the towel. Hold 5 seconds
Lower your leg to the starting position and repeat 10 times.
All photos with kind permission of ©Physiotec™
Once these exercises become easier your physiotherapist will start to progress you on to more functional exercises like sitting to standing and squatting
When can I return to normal activities?
When can I start driving again?
It is always good to check with your insurance company however, we advise it should be safe to return to driving when:
- You can walk comfortably without crutches
- You have good pain free movement in your knee joint
- You can perform an emergency stop
What about hobbies/sport?
If you participate in an active hobby then it is advisable that you do not return to this until you have full strength, full range of movement and you can walk briskly without experiencing pain and swelling. It can take at least 6-8 weeks before you can return to your usual sports or activities but your physiotherapist can guide you on this depending on how well your rehabilitation is progressing.
If you play a sport, you will be advised to practice sports specific activities like dribbling or jumping. Build up these exercises gradually, in order to help regain strength and flexibility, before returning to full training sessions and competition.
Do I require further treatment?
Physiotherapy follow up
A formal physiotherapy referral will have been made for you. It is common following the first patella dislocation for it to reoccur and so it is very important that you follow physiotherapy advice. These sessions will enable you to regain full range of movement and strength, stabilise the patella and return to full function.
If you have not received an appointment one week after receiving the call, please contact the physiotherapy department on 01482 674880 between the hours 8.00am – 4.00pm Monday to Friday. If there is no answer please leave a message and your call will be returned with the same working day.
Fracture Clinic follow up
A follow up appointment is not required in fracture clinic and you have been placed on a Patient Initiated Follow Up (PIFU) pathway. This means you will not have another appointment to be seen in fracture clinic.
If, however you have any problems or further queries relating to this injury within the next six weeks, you can contact us on 01482 674378 during clinic hours 9.00am – 4.30pm Monday to Friday. Please do not choose an option and when prompted leave a message if there is no answer and we will aim to get back to you within the same working day. If you have not needed to contact us in the six weeks after your injury, you will be discharged and should seek advice from your GP.
This leaflet was produced by the Orthopaedic Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in May 2025
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

