- Reference Number: HEY-886/2023
- Departments: Pain Medicine
- Last Updated: 29 September 2023
Introduction
This leaflet has been produced to give you general information about the Pain Management Programme. This leaflet should have answered most of your questions. It is not intended to replace the discussion between you and the healthcare team but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
The aim of the Pain Management Programme
There is no cure for chronic pain but a Pain Management Programme (PMP) can help each individual person manage their pain effectively. The aim of the PMP is to break the pain cycle that many patients find themselves in. Cognitive Behavioural Therapy (CBT) is a method of looking at a person’s thoughts, feelings and behaviours. Each of these influences the other and pain plays its own role in this process.
When we have pain, we may reduce activity to reduce the pain. When we stop doing the things we love we can sometimes feel low. In turn our thoughts can become negative and it can be more difficult to cope with the pain. It is important to understand all these elements have a role in effectively self-managing pain.
When and where?
The programme will consist of a series of appointments with a professional such as a nurse, physiotherapist or psychologist. The appointments will either be face to face or over the phone at a pre-arranged time.
What does the programme consist of?
The programme concentrates on both the physical and the psychological aspects of pain management. This is because pain involves both the mind and the body and for maximum effect they need to be tackled together.
A key factor for seeing improvement with the programme is your personal engagement with the principles of the programme and engaging with modifications in lifestyle to build on your personal coping strategies.
Strategies that we might cover in the Pain Management Programme.
Goal setting
Setting realistic goals will help to build strength and confidence. Small achievable goals are set to start with, which then build to larger goals. Goals can be changed according to a person’s needs.
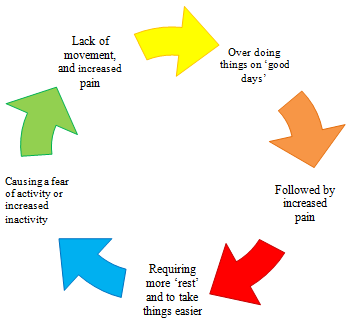
Pacing
Pacing is a method of balancing activity and rest. By balancing activity and rest you are able to slowly build up what you are able to do increasing strength and stamina. When we have a good day we tend to “overdo” it. We then have more pain/ fatigue in the following days. This is called the boom bust cycle. In this cycle the pain is controlling the person’s activity. By using pacing the person is able to break the cycle to achieve more activity with less pain.
Flare up plan
A flare up of pain is a period of uncontrolled pain. There is not always an identifiable cause of the increase in pain. As part of the programme you will be shown how to develop your own “flare up” plan which you can use to guide you when your flare ups occur. The more effective the pain management, the less the flare ups will occur, the shorter they will last and the less severe they will be.
The benefit you gain from this course will depend on how much you put into the programme. It can be hard work and a difficult challenge to face at times but the staff are there to guide you through the process. We will not be focusing on one specific area of pain but will be looking at what you can achieve in spite of the pain.
Objectives of the programme
- To increase knowledge and understanding of pain
- To develop an effective personalised flare up plan
- To increase self-confidence
- To promote self-help
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

