- Reference Number: HEY-026/2023
- Departments: Upper GI
- Last Updated: 1 November 2023
Introduction
This leaflet has been produced to give you general information about your operation. It explains what is involved and what the risks are. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss your concerns with a member of your healthcare team.
What is an Oesophagectomy?
The oesophagus (gullet) is a muscular tube, which allows food to travel from your mouth to your stomach. The aim of this surgery is to remove the diseased part of the oesophagus. This may involve removing all or part of your oesophagus, and sometimes part of the stomach, depending on the size and location of the diseased section. The name of the operation is an Oesophagectomy (sometimes also called Oesophagogastrectomy). This operation is performed if you have an ulcer or growth which needs to be removed because of the problems it is causing. The ulcers or growths are often caused by cancer, but not always.
Are there any alternative treatments?
Surgical removal of the gullet is currently the only known way of curing oesophageal cancer. It is often used in addition to other treatments such as chemotherapy or radiotherapy. Your surgeon will have discussed with you whether you will require a course of chemotherapy before having surgery. This is known as ‘neo-adjuvant chemotherapy’ and its aim is to reduce the size of the cancer. Some patients also go on to have further chemotherapy after surgery. This is known as ‘adjuvant chemotherapy’ and its aim is to ensure that there are no remaining cancer cells. Not everyone is suitable for or needs this treatment, so do not worry if you are just having surgery.
Alternatives to surgery are:
- Chemotherapy and / or radiotherapy
- Oesophageal stenting
- Palliative care
If surgery is not an option, the alternative treatments will be discussed further with you in more detail.
What happens before the operation?
Before your operation, it is important that you stay as fit and well as you can. If you smoke cigarettes, it is vital that you try to stop immediately. This will help reduce your risk of getting a chest infection after surgery.
Taking regular, gentle exercise and eating well is very important. If swallowing is becoming more difficult before your operation, ask your GP to refer you to a dietician or contact the clinical nurse specialists, whose contact details are at the back of this leaflet. This is very important if you can only manage liquids.
You will receive an appointment or phone call asking you to attend for a Pre-assessment. This is to assess your general health and fitness for the operation. You may be asked some medical questions and a number of routine tests may be performed. For example, blood tests, electrocardiogram (otherwise known as an ECG or heart tracing), chest X-ray and lung function tests.
It is very important that you bring any medicines, tablets or inhalers that you are taking.
Preparing for your operation
- You will usually be admitted to the ward the day before your operation and be seen by a member of the surgical team. If there is anything that you have not understood, have forgotten or are particularly worried about, now is the time to ask before you sign the consent form.
- A general anaesthetic is used for this operation, which means you will be asleep during the operation. The doctor who gives you the anaesthetic is called an anaesthetist. They will visit you to discuss the type of anaesthetic to be used and answer any questions you may have about this.
- Anti-embolic stockings will be applied to help reduce the risk of a deep vein thrombosis (otherwise known as a DVT or blood clots in the legs). You may be given a small injection, just under the skin in your stomach to help prevent a blood clot.
- You will not be allowed to eat or drink anything for between 4 – 6 hours before surgery. A porter and a ward nurse will take you to theatre and a relative may go with you and wait until the anaesthetist is ready.
What is involved in the operation?
There are different ways of doing this operation. Usually this is performed by “keyhole” surgery, which requires a number of small cuts in the stomach and the right hand side of the chest, and a cut in the neck. If keyhole surgery cannot be performed, there may be 2 larger cuts, one down the middle of your stomach and the other either on your chest or above the collarbone. In some people, all 3 cuts are required. Your surgeon will have discussed with you which surgical approach is most likely to be used. The operation can take between 5 – 8 hours.
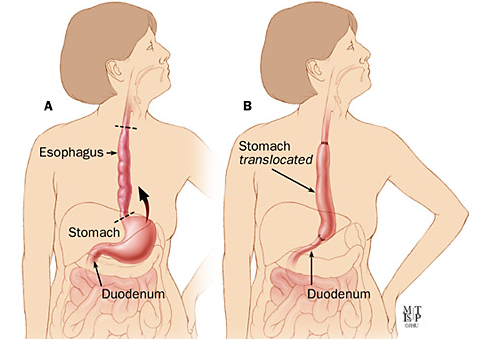
During the operation, most of your oesophagus and a small part of your stomach will be removed, along with the lymph glands, and the remainder of the stomach is made into a tube. This tube is joined to the remainder of the oesophagus, either in the chest or high in the neck, through the neck wound (fig A)
Fig A
The area that has been removed will be sent away to be looked at under the microscope. This helps to decide whether you will require any further treatment. The precise details of your own operation will be discussed with you by your Consultant Surgeon. This operation is major surgery. Occasionally, during a planned operation on the gullet, your surgeon may find the disease is not suitable for surgery, perhaps because the cancer cannot be removed as it is more advanced or has spread to other organs. If this is what happens in your case, other types of treatment will be discussed with you.
How long will I be in hospital?
It is important that you and your family, together with your nurses, make plans as early as possible for going home. This helps to ensure that you do not have to stay in hospital longer than necessary. You should expect to stay in hospital for around 10 days to 2 weeks. However, rates of recovery from this surgery vary from person to person, and are dependent on several things. Up to half of the people having this operation can develop a “complication”, which may increase their length of stay in hospital. Your risk of developing a complication will be explained to you in more detail by your surgeon and clinical nurse specialist.
Risks can include:
- Chest infections and other respiratory (lung) problems
- Wound infections
- Anastomotic leak (delayed healing of the new “join” between oesophagus and stomach)
- Heart problems
- Deep vein thrombosis (blood clot in the veins of the leg)
- Damage to the nerves of the voice box
What will happen after my operation?
It is usual to spend up to a few days on the intensive care unit, after your operation. You will then be cared for on Ward 14.
You will be awake and able to talk on arrival to the intensive care unit but will probably be quite sleepy. You are likely to have hazy memories of this time, some patients experience vivid dreams and hallucinations. Some people can find these disturbing, but they are only temporary. You will be attached to various tubes and monitors, which allow regular recordings of your observations. This can seem a little frightening but it helps to know what they are all for.
These may include:
- An oxygen mask that fits over your nose and mouth, and ensures you receive sufficient oxygen to help you recover from the anaesthetic.
- Intravenous fluids (a drip) are usually given by a thin tube that is placed in the vein at the side of your neck (central line). This prevents you from becoming dehydrated while you are ‘nil by mouth’. Antibiotics may be given in the same way. These will be stopped when you are drinking normally.
- A catheter (tube into your bladder) will allow the nurses to accurately record your urine output and means you will not have to get out of bed to pass urine. This will be removed in a few days once you are mobile.
- A naso-gastric tube (NG tube) which goes up a nostril, down the back of the throat and into the stomach will be used to help relieve sickness and also to aid the area of the operation to heal. It usually only stays in a few days.
- Intercostal drains (chest drains) are inserted through your chest wall to allow fluid which may have collected around the lungs, to drain away. They usually stay in for the first 2 – 4 days.
- Abdominal drains (Robinson’s drains) are inserted through the abdominal (tummy) wall. It helps you to heal by draining fluid away from the area of the operation. These stay in for a few days.
- A feeding tube (jejunostomy tube) may be inserted into your small bowel at the time of surgery to allow feeding directly into the bowel. This is to allow the join between your remaining oesophagus and stomach tube to heal. This can be in place for up to 7 days.
- You will not be allowed to eat or drink anything for a few days. You may then have a special X-ray called a gastrograffin swallow. This is to check that the join is healing. The x-ray involves drinking a clear liquid. If the X-ray shows that the join has healed, then the naso-gastric tube will be removed, and you will be able so start drinking by mouth. Over a period of 48 hours you will continue to increase your intake by mouth to include food. During this period, most of the drains and tubes will have been removed. If, however, the X-ray shows the join has not yet healed, then you will remain nil by mouth for a longer period of time and the test will be repeated.
- An epidural may be inserted through your back for pain relief to be delivered.
- A PCAS (patient controlled analgesic system) may be used to give you strong pain relief medication either through your epidural or intravenous drip.
- You may wake to find flotron boots around your lower legs. These pump up and down to encourage blood flow and prevent blood clots forming in the legs.
- Your wounds will depend upon whether you have had keyhole or open surgery. If keyhole surgery is performed, you will usually have a number of small cuts on your abdomen (tummy) and chest, and a cut to the left side of the neck.
- If open surgery is performed and then there may be a large cut down the middle of the abdomen, and another either on your chest, or above the collar bone. Types of skin closure vary, this will be discussed further with you.
How quickly will I recover?
Recovery from a major operation involving the digestive organs is not fast. It can take months for the digestive system to adapt after surgery, although some patients do recover quicker than others. A physiotherapist will teach you important coughing and breathing exercises, which you will be encouraged to do after your operation. These exercises will help your lungs re-expand and prevent serious chest infections. They will also advise you regarding mobility, which will help prevent the formation of clots in your leg.
Your food and drink intake will be closely monitored by a dietitian and advice will be given to help you eat well. Your feeding tube (jejunostomy tube) to maintain calorie intake may still be in place at this point. This may continue for 2 – 4 weeks after discharge. You and your family will receive training in this and a district nurse will be arranged before discharge to support you at home if needed.
During this recovery period you will have regular visits from your clinical nurse specialist. This is to ensure you and your family continue to have their support and to provide further discharge information in the form of “A Guide to Life After Oesophageal Surgery” produced by the Oesophageal Patients Association.
What can I expect when I go home?
Thinking about going home can be quite an anxious time. It is likely that you and your family will have concerns about how you will manage and what to do if problems arise. You should already have the contact details of your clinical nurse specialist, whom you should contact with any queries or concerns.
Your consultant will arrange to see you in the outpatients department a few weeks after discharge. If you do not receive this appointment, contact your clinical nurse specialist who will arrange one for you. This appointment is to review your progress and monitor your weight. They will also discuss the pathology findings from the area of gullet and lymph glands which were removed at the time of the operation. Further treatment options, if necessary will be discussed at this appointment.
Your wounds will be healing by the time you leave hospital, however you may still have some bruising, swelling and numbness; this is quite normal and may take some weeks to improve. Should your wound become red, hot to touch or ooze fluid, please inform your district nurse as soon as possible so that it can be reviewed.
You may take a bath or shower as normal, using unperfumed soap and pat your wounds dry.
You may continue to feel tender around your wounds for some time after you go home. The amount of discomfort experienced varies between individuals, you can expect to feel some discomfort for up to 3 months after your operation. You will be given pain relief medication to take home and you will need to see your GP for further prescriptions. Continue to take your pain relief medication on a regular basis, especially in the first week after discharge. When you feel ready, reduce them gradually over a number of days.
It is important to continue the exercises taught by the physiotherapist regularly once you are at home and you must avoid heavy lifting or strenuous exercise for at least 8 weeks. This allows the wounds to heal properly. It is important to try and develop a routine and take gentle exercise like short walks. It takes up to 6 months to recover fully from this operation, so build up to normal activities in your own time.
After a major operation it is not unusual to feel low in mood. This may be related to a number of factors such as lack of energy and the frustration of the impact an operation can have temporarily on jobs, hobbies, relationships and sex drive.
It is important to remember that it can take a few months until you feel you have regained some or most of the strength and energy that you are used to. Getting plenty of rest in the early days of being at home is important. Having an afternoon nap for the first few weeks is recommended and will prevent you from becoming overtired.
You may plan a holiday as soon as you feel ready to travel. Holidays involving flying should not be taken for approximately 6 – 8 weeks after surgery. Check with your consultant and insurance company prior to flying.
You may be able to start driving approximately 6 – 8 weeks after surgery, once you are able to perform an emergency stop, without pain or hesitation. Check with your consultant and with your insurance company prior to driving.
Will I be able to eat normally?
In the weeks following surgery, you might lose weight but things will slowly improve as your appetite and confidence improves. Although initially you may not feel like eating, especially as you will still be having overnight feeding via your feeding tube, it is very important that you try. Starting to eat normal foods can feel strange at first, you are likely to feel full very quickly and have a loss of appetite.
A dietitian will visit you on the ward prior to going home to advise you on how to overcome some of these problems. You will also be provided with nutritional supplements, if necessary, to ensure sufficient calorie intake.
Eat ‘little and often’. As you will feel full quickly it is important to eat several small meals and snacks throughout the day, rather than rely on 3 small meals a day. To help with loss of appetite, concentrate on eating the foods and snacks you enjoy. You should not need to avoid any particular food, however you may find certain foods upset you in the early days. It may be helpful to keep a food diary and discuss this with your dietitian if this occurs.
It is important not to drink too much with your meal, but equally it is important to sip fluids with your meals to aid the passage of food through your new gullet. It is NOT necessary to stay on a liquid diet.
Sometimes oesophagectomy patients find that food can ‘stick’ on its way down and swallowing becomes a bit difficult. However, it is important to persist with eating if this does happen, as things often improve as you begin to eat normally. If your swallowing does not improve again, it can mean that the join between your new gullet and stomach has narrowed down a little. If this happens and your swallowing becomes difficult, contact your clinical nurse specialist, who will be able to advise you. Some patients who have had an oesophagectomy experience acid reflux or heartburn. This is caused by some of your stomach juices or bile coming into the back of the throat. This may happen if you lay flat on your back, eat too much before going to sleep, eat and drink too close together or bend over. It may be helpful to sleep with extra pillows, put bricks under the head of the bed and try not to eat late in the evening. You may have been given anti acid medication to try and prevent this. If this becomes a problem contact your clinical nurse specialist.
As you get used to eating again, you may find that you burp, feel sick or feel bloated. You may experience all of these symptoms at one time or another. This is quite normal after an oesophagectomy and is usually temporary. Medication may be used to help if this becomes a problem.
A sensation known as ‘dumping syndrome’ occurs when the food you have eaten passes rapidly through your system, and may give rise to some of the following symptoms: dizziness, nausea, sickness, sweating, pain in the abdomen and occasionally fainting. Diarrhoea or frequent bowel movements may follow. It can be unpleasant and distressing but is not serious, generally the frequency of attacks become less and settle 2 – 3 months after surgery. It generally occurs half an hour or more after eating and the effects normally disappear in half an hour or so. The symptoms may be controlled by:
- Avoiding sugary drinks.
- Limiting the amount of sugar and sugary foods eaten (jam, honey, sweet cakes and biscuits, sweets, mints and chocolate, sugary cereals).
- Consider using artificial sweeteners in drinks instead. If you fancy something sweet it is best to have a small amount (i.e. one square of chocolate) and have this after a meal.
- Taking small well balanced meals containing some fat, protein and starchy foods (potato, bread, pasta, rice and cereal).
- Avoid alcohol.
A rare complication of oesophagectomy is damage to the nerves of the voice box. This can result in hoarseness of the voice or a sore throat. This is nearly always temporary and is due to bruising of the nerve. Very rarely, permanent damage is done, resulting in a change in quality of the voice.
When can I return to work?
The timing of a return to work depends on many factors: age, type of work and whether you have returned to your previous level of fitness. In any event, it may be some months before you do. Heavy work makes more demands and might not be suitable, especially if much bending or lifting is involved. Hopefully your employer may be able to help by using your skills and knowledge for lighter work, or arranging for you to start with a few hours a day (also known as a phased return). Remember to plan into your day to take nourishment when you need it – little and often.
How often will I have a check up?
After your initial post discharge appointment you will be followed up by the surgical team regularly for 5 years. Meanwhile, if you are concerned about any aspect of your recovery, you can contact your clinical nurse specialist.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Upper GI Clinical Nurse Specialists on telephone number (01482) 624349 or 624350
Useful Contacts
Macmillan Cancer Support – Provides practical information and emotional support for people living with cancer. Call 0808 808 00 00 Monday-Friday 9am-8pm or go online at www.macmillan.org.uk
Humberside Oesophageal Support Group – Offers support which is provided by local people who have been affected by oesophageal cancer. www.hosg.org.uk
Oesophageal Patients Association – For information and support from former patients. www.opa.org.uk
Welfare Rights – If you think you may be entitled to benefits or wish to ask advice, call telephone number (01482) 300300
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

