- Reference Number: HEY-136/2023
- Departments: Oral Surgery, Dentistry and Max Fax
- Last Updated: 31 July 2023
Introduction
This leaflet has been produced to give you general information about your condition. Most of your questions should have been answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a Neck Dissection?
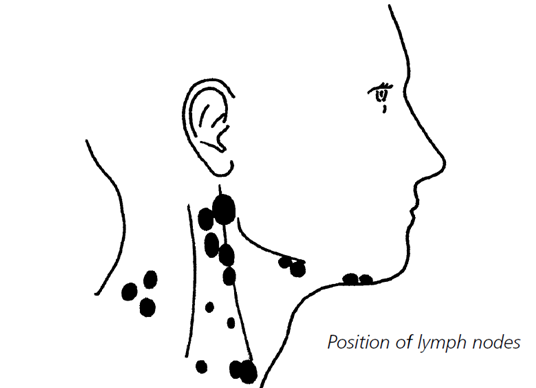
A neck dissection is an operation to remove lymph nodes from the neck on one or both sides (figure 1). Lymph nodes are present throughout your body. You may have felt swollen lymph nodes in your neck when you have had an infection such as a simple cold. Their job is to filter the liquid which naturally leaks out of blood vessels. This liquid known as lymph, travels from the tissues to the nodes which contain a lot of white blood cells, designed to trap and fight germs which can cause infection. As well as trapping germs the lymph nodes can also trap cancer cells.
Why do I need treatment?
If you have been diagnosed with cancer it is important to check if it is also in the lymph nodes. It is not often possible to tell this until after your operation when the nodes removed from the neck are carefully looked at under a microscope. Your doctor will have already felt your neck to see if there are any lumps and you may also have had a special scan (Ultrasound, CT or MRI) to look more closely at the nodes. They can feel big if there is infection in the area, so if you can feel a lump in your neck it does not necessarily mean that the cancer has spread. Also not all lumps in the neck are lymph nodes.
If there is only a small number of cancer cells present in the nodes then the neck can feel normal and appear normal on a scan. This is often why we do not know if the cancer has spread to the neck nodes until they have been looked at under a microscope.
Can there be any complications or risks?
There are complications and risks of this surgery and it is important that you are aware of these and have the opportunity to discuss them with your surgeon.
There are problems associated with the damage to the nerves:
- Accessory nerve – this is a nerve which runs from the top to the bottom of the neck and helps you to move your shoulder. The nerve has some key lymph nodes lying very close to it and so it is often bruised during a neck dissection. If the nerve is bruised it will stop working for several months. Is this happens you may experience pain and some difficulty in moving your shoulder, which makes getting dressed rather difficult, and also brushing the hair at the back of your head. Often the lymph nodes cannot be completely removed without sacrificing this nerve. Should this be the case then these shoulder problems will be permanent.
- The facial nerve: the branch of the facial nerve, which makes your lower lip move, can be bruised or sacrificed when the lymph nodes close to it are removed. If this happens then the lower lip does not move properly and you have weakness, which results in a crooked smile. If it is merely bruising or stretching the majority of patients recover but it can take several months to fully improve.
- Numb skin: The skin of your neck will be numb after the surgery. This will improve to some extent, but you should not expect it to return to normal.
- Stiff neck: You may find that your neck is stiffer after the operation. You may need further physiotherapy for your neck and shoulder, if they are affected. We may be able to make you an outpatient appointment for this near to your home.
- Haematoma: Sometimes the drain tubes which are put in during the surgery can become blocked or fail to work. This can cause blood to collect under the skin and form a clot (haematoma). If this happens, you may need further surgery to remove the clot and replace the drains.
- Chyle leak: (pronounced ‘kile’): Chyle is the name given to digested fats that are carried from the gut in the lymphatic system. Occasionally one of the lymph channels, called the thoracic duct, is damaged during a neck dissection, usually on the left side. This can be hard to spot during the operation. If this occurs, chyle can collect under your skin or may be seen in your neck drain. If you have a chyle leak you will usually be placed on a fat-free or modified fat diet for a period of time (usually 2-3 weeks) until the leak has healed, or you may be taken back to theatre to repair the leak. There is a small chance that we will need to feed you intravenously (through a small tube into a vein). This would mean we’d need to keep you in hospital longer than originally planned.
- Damage to the hypoglossal nerve: Very rarely this nerve (which makes your tongue move) also has to be removed, if it is affected by the tumour. If this is done, you will find it difficult to move food from that side of your mouth and it can also interfere with your swallowing. If this happens, you may need to eat and drink a modified diet (such as a soft or liquified diet).
- Your speech sounds may also be less clear if this nerve is affected. The Dietitian and Speech and Language Therapist will help to support you and offer advice.
How do I prepare for the operation?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
You will be given a letter detailing where you should attend, starving instructions and the time to report to the ward. Staff will greet you and show you around the ward. You will be seen by the doctor and possibly the anaesthetist. The type of anaesthetic you will be having is called a general anaesthetic. You will be prescribed pain relief medication to manage any pain you may suffer following the operation.
You may be required to attend a pre-assessment where the nurse will prepare you for the surgery and you can ask any questions you may have. She will also ensure you are fit for the anaesthetic.
What will happen?
Except when radiotherapy is going to be used as the main treatment for the primary disease, or unless the primary disease has already been successful treated, a neck dissection is usually carried out at the same time as the operation to remove a cancer from around the face or mouth. It will therefore take place under the same general anaesthesia.
A large incision is required to gain access to the lymph nodes in the neck. The cut usually starts just underneath the chin and extends downwards towards the collarbone before arching upwards to end behind the ear. Skin flaps are lifted off the tissues of the neck to expose the underlying tissues containing the lymph nodes. These are removed together with the tissues that might contain tumour. Once the operation is complete drains are put in place to prevent a build-up of fluid, the skin flaps are replaced and held with stitches or clips.
What happens afterwards?
The tubes used as drains usually stay in place for five to seven days before being removed. Any discomfort is usually short lived. It is necessary to make sure that the incision heals without any infection and so you will be given antibiotics whilst you are in hospital. You will also be given regular pain relief medication. The skin stitches or clips will be removed about a week following surgery.
You may have to have further treatment after your neck dissection; however this depends on what is found when the lymph nodes are looked at under the microscope. It takes several weeks to look at the lymph nodes properly and so your doctors will not know until then whether additional treatment is necessary.
Should you require further advice, please do not hesitate to contact the Maxillofacial Department (01482) 463218
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

