- Reference Number: HEY-1348-2022
- Departments: Orthopaedics
- Last Updated: 1 December 2022
Advice regarding healing and recovery
Introduction
This leaflet has been produced to give you general information about your injury. We understand you may not have seen a clinician face to face in fracture clinic however, most of your questions should be answered by this leaflet. If after reading it, you have any concerns or require further explanation, please do not hesitate to contact the fracture clinic team. Contact details are available at the end of this leaflet.
What does a minor avulsion fracture or no fracture seen mean?
Following your virtual fracture clinic review you have been diagnosed with a minor foot injury. As a result is it likely that you have sustained an injury to the soft tissues in your foot. On occasions, an avulsion fracture may be reported but a ligament pulling away a small piece of bone as it is stretched usually causes this. Avulsion fractures can be treated as a soft tissue injury and do not usually require immobilisation.
How should it be treated?
Minor foot injuries can be treated simply in a tubigrip and you can place as much weight through the foot as you find comfortable with or without the help of crutches.
In some circumstances you may have been offered a removable slipper cast which can be removed when in bed, to exercise the ankle and for hygiene purposes. The cast can be walked on with or without the use of crutches.
To manage your pain, we advise that you regularly take simple pain relief, which can be bought over the counter. If you have allergies or conditions, which prevent the use of pain-relieving or anti-inflammatory medication, please seek advice from your doctor or a pharmacist.
Once you can walk comfortably without the cast, it should be discarded. This should be no later than 3 weeks after its application.
What should I do in the first few days?
Controlling the pain and swelling by following the principles of RICE are important:
R REST
Complete rest is not advisable. If necessary, you will be given crutches to help you take some weight off the injured foot. Exercises in the section below, can be started straight away.
I ICE
Ice will help reduce the pain in your foot and so should be applied for 10 – 15 minutes before performing any exercises. This will also help to reduce the swelling.
There are many different ways in which ice can be applied however crushed ice, in the form of frozen peas for example, is the most effective. Whichever method you choose it is important that you wrap the ice in a damp towel, in order to prevent it from ‘burning’ the skin.
Please Note:
- Only use an ice pack on areas that have normal skin sensation i.e. where you can feel hot and cold
- Do not apply ice to an open wound
- Do not apply an ice pack to an area that has poor circulation
- When you apply ice to your skin, check the skin every five minutes and stop using it if:
- the area becomes white, blue or blotchy
- the area becomes excessively painful, numb or tingles
C COMPRESSION
If you have been given a tubigrip to wear it is important this is removed if you develop any signs of poor circulation such as tingling, numbness, blueness of the skin of the foot and increasing pain. The tubigrip should be removed when you go to bed at night, as when you are asleep you cannot monitor these symptoms.
E ELEVATION
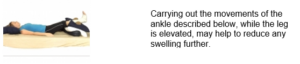
The leg should be elevated above the level of the heart as much as possible, as this will reduce and prevent swelling.
What exercises should I do?
The simple exercises described below will help prevent stiffness developing in the ankle and foot.

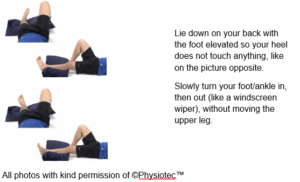
2. Ankle inversion and eversion
How long will the pain and swelling persist?
Pain and swelling can persist for 3 months following the injury. We advise continuing the use of simple analgesia such paracetamol to allow you to walk normally. Swelling is usually worse towards the end of the day. If this does occur, continue to use elevation as described previously.
When can I start driving again?
It is always good to check with your insurance company however we advise it should be safe to return to driving when:
- You are no longer using a plaster slipper
- You can walk comfortably
- You can perform an emergency stop
When can I start increasing my activity?
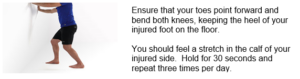
Once you are able to walk normally, you should gradually increase your level activity. Consider trying the following exercises.
- Stand facing a chair and step backwards with your injured foot.
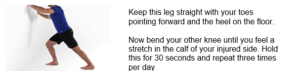
2. From the position in exercise one move your injured foot forward but keep it slightly behind your other leg.
3. Stand holding on to a chair, spread your weight equally over both feet and push up onto your toes as high as possible.

4. Stand on your injured leg and balance for as long as possible. To begin with, you may need to hold on to something solid to prevent you falling over.
All photos with kind permission of ©Physiotec™
If you participate in an active hobby then it is advisable that you do not return to this until you have full strength, full range of movement and you can walk briskly without experiencing pain and swelling.
If you play a sport, you can practice sports specific activities; like dribbling or jumping. Build up these exercises gradually from around 6 weeks, in order to help regain strength and flexibility, before returning to full training sessions and competition.
Do I require a follow-up?
Do I need to be referred to Physiotherapy?
If the fracture clinic team feel you need to be seen by the Physiotherapy team, you will be directly referred to physiotherapy from fracture clinic and if this is the case, you will have been informed of this in your telephone call following your Virtual Fracture Clinic appointment. You will receive a letter or phone call to book this appointment within 2 weeks of the referral being made.
If you have not received one within this time, please contact the physiotherapy department on 01482 674880 between the hours 8.00am – 4.00pm Monday to Friday. If there is no answer please leave a message and your call will be returned with the same working day.
Most of the time however, a referral to Physiotherapy is not needed, but if you have any concerns, are unable to follow the advice in this leaflet, or if you still have reduced movement, strength or function, East Riding GP patients can contact the East Riding MSK Physiotherapy service on 01377 208300. Alternatively you can complete a self referral form on https://www.chcpmsk.org.uk/self-referral-form-introduction
Hull GP patients should call the fracture clinic number in the information below.
Do I need a Fracture Clinic follow up appointment?
A follow up appointment for fracture clinic is not required and you have been placed on a Patient Initiated Follow Up (PIFU) pathway. This means you will not have another appointment to be seen in fracture clinic.
If, however you have any problems or further queries relating to this injury within the next six weeks, you can contact us on 01482 674378 during clinic hours 9.00am – 4.30pm Monday to Friday. Please do not choose an option and when prompted leave a message if there is no answer and we will aim to get back to you within the same working day. If you have not needed to contact us in the six weeks after your injury, you will be discharged and should seek advice from your GP.
This leaflet was produced by the Orthopaedic Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in May 2025
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

