- Reference Number: HEY-602/2021
- Departments: Emergency Department, Orthopaedics
- Last Updated: 19 January 2021
Introduction
This leaflet has been produced to give you general information about the symptoms and management of your injury. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a mallet finger?
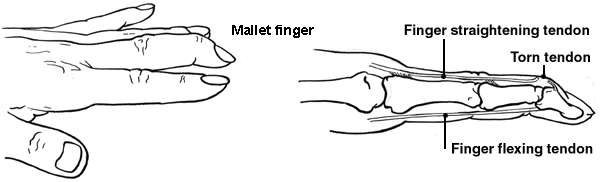
A mallet finger is where the tip of your finger becomes bent towards your palm and you are unable to straighten it and you may experience swelling and pain.
It is usually caused by an injury to the end of the finger which causes it to bend further than normal. This results in a tear of the tendon that would usually straighten the end of the finger.
Reproduced with the kind permission of Patient.co.uk
Sometimes the tendon will not tear but a small piece of bone it attaches to will be pulled off the finger. The result will be the same as the tendon is unable to pull on the bone.
How is it treated?
A splint is usually fitted for you to wear which will keep the tip of your finger fully straight. It must be worn day and night for up to 8 weeks. This allows the ends of the tendon/ bone to stay together and heal.
You will be contacted with an appointment with a member of the hand therapy team within 3 working days. If you do not hear from them within this time please contact the physiotherapy admin team on (01482) 674880 and this appointment can be arranged for you.
Your splint should only restrict movement at the top joint and not at the middle joint of the finger. It is important you continue to move the middle joint but do not remove the splint. Perform this exercise 10 times, 3 to 4 times per day.
It is important that the splint is removed for washing but you must ensure the finger remains straight at all times. To do this lay your hand palm down on a flat surface and slip the splint off. Wash and dry the finger thoroughly whilst the hand remains on the flat surface and then slide the splint back on.
If you find, as the swelling settles, your splint becomes too large for your finger contact your Therapist to discuss.
If you do not comply with the use of the splint and the length of time it should be worn then it is likely that the ability to straighten the end of your finger will not return.
Pain relief
To manage your pain it is advised that you regularly take simple pain relief medication which can be bought over the counter. If you have allergies or conditions which prevent the use of pain relieving or anti-inflammatory medication, please seek advice from a pharmacist or your doctor.
Is there anything I should avoid?
- Do not try to examine how much your finger has healed by bending it.
- Do not wear rings on the affected finger. If the finger is swollen it may well affect your circulation and interfere with the healing process.
- Do not consume alcohol, massage the injured area or apply heat as all can be detrimental in the early stages of healing.
- Please note that smoking may delay healing
Outcome
Some patients may be left with a slight bend in the finger, however this will not usually affect the function of the finger and no further medical input is required.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

