- Reference Number: HEY-395/2019
- Departments: Physiotherapy
- Last Updated: 19 February 2019
Introduction
This leaflet has been produced to give you general information about your condition. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is Malignant Spinal Cord Compression (MSCC)?
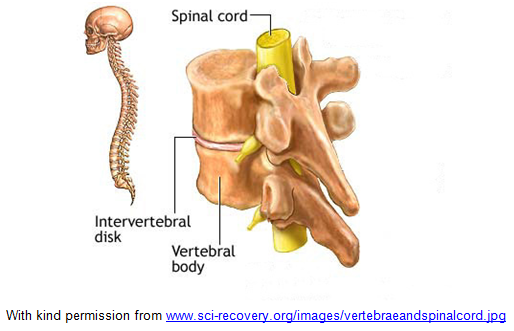
The spinal cord is a large bundle of nerves that runs down the length of the spine. The spine is made up of individual bones called vertebrae which help to keep the body upright and protect the spinal cord. As the spinal cord passes through each bone it gives off smaller nerves called nerve roots. These supply the trunk, arms and legs with sensation (feeling) and control of muscles. The spinal cord carries messages between the brain and the rest of the body.
Spinal cord compression is due to pressure on the spinal cord and its nerves. This results in swelling and a reduction in the blood supply to the spinal cord and nerve roots. This can be due to the bones being affected by cancer causing them to weaken; the cancer spreading into the tissues around the spine or the cancer affecting the spinal cord itself.
Spinal cord compression can be caused by a primary tumour (original tumour) or due to secondary spread from metastases (spread of the tumour to other parts of the body away from the original site). Metastases are the most common cause of MSCC.
Spinal cord compression is more commonly seen in people with cancer affecting the breast, lung, or prostate and in people who have lymphoma (cancer of the lymphatic system, part of the immune system) or myeloma (cancer of blood plasma cells, found in the bone marrow).
What symptoms will I have?
This depends on the part of the spinal cord affected by the tumour but can consist of:
- Unexplained pain in the neck or back, may feel like a ‘band’, sometimes described as burning or shooting pain. It can spread (radiate) around the side of the body or down the arms or legs
- Numbness, tingling or pins and needles in the arms or legs
- Loss of control of the bowel and bladder (constipation, loose stools, problems passing urine)
- Weakness in the arms or legs
- Feeling unsteady on your feet, difficulty walking, or your legs giving way
How is malignant spinal cord compression diagnosed?
Usually an MRI (Magnetic Resonance Imaging) scan is used to diagnose spinal cord compression. This involves lying on a bed inside a long tube for about 30 minutes whilst magnetic fields are used to produce a detailed picture of your body. It is not painful but it is noisy and some people can feel a little claustrophobic. Pain relief (analgesia) may be given before this procedure if you find it uncomfortable to lay flat.
Sometimes you may have an X-ray taken or a CT (Computerised Tomography) scan. This takes a series of X-rays to build up a 3D picture of the inside of your body. Bone scans can check if there are any abnormal areas in the bone but they cannot diagnose malignant spinal cord compression.
What medical treatment will I have?
Treatment should be started as soon as possible after diagnosis, in order to prevent permanent damage to the spinal cord, which can lead to serious disability including paralysis (inability to move or feel).
The choice of treatment depends on several factors, including the type and stage of cancer, the area affected, previous treatment and your general health and fitness.
Your healthcare team will discuss your treatment options, giving you details about the possible benefits and risks of particular treatments and involving you in all decisions about your treatment and care. You can ask any questions you wish and can change your mind as your treatment progresses or your condition or circumstances change.
Bed rest
You may be asked to stay in bed, lying as flat as possible. This is the safest and most supportive position for your spine. You may need to wear a supportive collar if your neck is affected. If your doctor considers your spine to be stable you will be able to sit up, if this causes discomfort please inform the doctor or nurse immediately.
Supportive care
The nursing team will help assist with personal care, such as washing and toileting. Sometimes a urinary catheter is needed to help empty your bladder or medicines may be offered to improve bowel function. They will also help to keep you comfortable in bed and assist you with meals if needed.
If you are having surgery or are unable to move around you may be required to wear white compression stockings and take certain medicines that help to reduce the risk of blood clotting (anti-coagulants).
If you are unable to move around you are at risk of developing a pressure sore and so may be offered a pressure mattress or cushion. You will also be encouraged or helped to change position and participate in gentle exercises/movement to ensure that your skin remains healthy.
Pain Relief
Medicines are available if you have any pain.
Steroids
Steroids (called dexamethasone) are usually given to reduce the swelling around the nerves. These are gradually reduced over time.
Surgery
Sometimes surgery may be considered for a small number of people as part of their treatment. This will be discussed with you. If you agree to this procedure you will be transferred to the care of a neurosurgeon. The aim of surgery is to remove as much of the tumour as possible which relieves pressure on the spinal cord. This may involve removing part of the bones that make up the spine. Treatment may involve injecting special bone cement into the vertebrae to strengthen the spine or using metal rods or bone grafts to further stabilise the spine.
Radiotherapy
Radiotherapy is the usual treatment for MSCC. This involves using a machine called a simulator to assist in accurately marking on your body where the radiotherapy needs to be delivered. You have to lie on your back and have X-rays and measurements taken. A different machine, called a linear accelerator, is used to deliver the radiotherapy treatment; this again involves lying still on a firm couch for a few minutes whilst the treatment is delivered.
High energy X-rays are used to reduce the size of the tumour, thereby reducing pressure on the spinal cord. This treatment cannot completely remove the tumour and cannot achieve a cure, but aims to improve symptoms of pain and can sometimes stop the weakness developing further. Unfortunately there is not a good result in all cases especially if the nerve damage is severe with marked loss of function.
Radiotherapy usually involves 1 – 10 daily treatment sessions and can take several weeks to fully take affect. The return of some strength or sensation in the first week is an encouraging sign. No change in the first week means that recovery is unlikely.

Image taken from the Radiotherapy Department at the Queen’s Centre for Oncology and Haematology, Castle Hill Hospital
Are there any side effect to the treatment?
Sometimes radiotherapy treatment can cause nausea and sickness. This can often be prevented by taking an anti-sickness tablet. Treatment to the upper spine (chest area) may cause temporary soreness of the gullet or a sore throat if the neck is treated. Some people can feel extremely tired during and after their treatment.
Chemotherapy
Chemotherapy is occasionally used to treat spinal cord compression. It may be used for tumours that are sensitive to chemotherapy such as lymphoma and small cell lung cancer. It uses anti-cancer (cytotoxic) drugs to destroy cancer cells.
Bi-phosphonates
These medicines help to relieve pain and protect the bones in your spine.
Hormone therapy
Hormone therapy is sometimes used in combination with other treatments such as chemotherapy. This may be used for MSCC when the primary tumour site is the breast or prostate.
What happens if I do not have any treatment?
If left untreated spinal cord compression would lead to permanent damage and paralysis, so it is important that it is recognised and treated promptly.
Who may be involved in my care?
- The Medical Team
- The Nursing Team
- Radiotherapy Department
- Physiotherapist
- Occupational Therapist
- Social Worker
- Specialist Nurse
- Psychological and Spiritual Support Services
The healthcare team is there to support both you and your family/carers to adapt to your individual situation. They can provide information and advice. The healthcare team aims to work with you to retain as much of your independence as possible, considering your individual wishes and needs. Information on how to access psychological and spiritual support will be offered if you or your family/carers need it.
What can I expect after my treatment has finished?
MSCC affects each person differently, some patients may be able to walk without assistance but for others they may continue to have reduced function and require a walking aid or wheelchair to keep their independence. The healthcare team will work with you and your family to organise a plan of care and rehabilitation to suit your needs.
The medical team and physiotherapist will decide when it is safe for you to start to sit up/get out of bed. This will be done carefully and gradually, closely monitoring for any signs of nerve symptoms, such as altered sensation and weakness or any increase in pain.
Sometimes it is necessary for patients to move from the cancer centre back to their local hospital to continue rehabilitation. This also makes it easier to plan for any support or equipment which may be needed on discharge.
The physiotherapist and occupational therapist (OT) will assess your ability to carry out daily tasks and activities. They will provide advice and support to help you adapt to your situation and to do as much for yourself as possible. They will also help to support you, your family members and carers when planning for your discharge from hospital.
The physiotherapist will teach you exercises to help build strength and prevent joint and muscle stiffness. They will also encourage breathing exercises to keep your lungs healthy and prevent chest infections.
Both the occupational therapist and physiotherapist will advise on any equipment that might be needed to help you with your daily activities and roles and to become mobile. The occupational therapist may offer to carry out a visit to your home in order to give appropriate advice on any equipment or adaptations that may be helpful to make it easier for you for the immediate or longer term future.
Some people may be offered further specialist rehabilitation if there is potential to further improve mobility and function. This may be provided within their own home or at a rehabilitation unit, or on a rehabilitation ward. Not all people would benefit from this but all patients would be assisted to improve their quality of life through adaptations to functional tasks.
The social worker may be involved with your care if you need to discuss having additional care support at home or are considering ongoing care in a residential or nursing home. They can also advise on any benefits you are entitled to e.g. disability living allowance, attendance allowance, carers allowance, car badge scheme.
The nurses and therapists will provide support and training for families and carers so that they can feel confident in supporting you once you are discharged from hospital, including use of any necessary equipment.
If you are returning home community based support will be offered, this may include nursing care, therapy and palliative care (such as support from Macmillan, District Nursing, Marie Curie, Specialist Palliative Teams or the Hospice). Palliative care involves treatments for pain relief, and practical and emotional support to help manage your condition.
Could malignant spinal cord compression occur again?
Unfortunately in some cases MSCC can come back, possibly affecting a different part of the spine. Contact your doctor or medical team if any of the symptoms listed previously in the leaflet return or worsen.
GLOSSARY (What do those words in the leaflet mean)?
- Analgesia – Pain relief medication
- Anti-Coagulants – Medicines that help to reduce the risk of blood clotting
- Bone Scans – Scans that check if there are abnormal areas in the bone
- Chemotherapy/Cytotoxic Drugs – Anti-cancer medication that destroys cancer cells
- CT – Computerised Tomography, is a scan that takes a series of X-rays to build up a 3D picture of the inside of your body
- Linear Accelerator – The machine used to deliver the radiotherapy
- Metastases – Spread of the tumour to other parts of the body away from the original site
- MRI – Magnetic Resonance Imaging, is a scan that uses magnetism to build up a detailed picture of areas of your body
- Nerve roots – Smaller nerves that come off the spinal cord at the level of each spinal bone
- Paralysis – Inability to move or feel
- Pressure ulcer – Skin sore that develops due to prolonged pressure on a body area
- Primary Tumour – Original Tumour
- Radiotherapy – High energy X-rays used to reduce the size of the tumour
- Simulator – A machine that assists the team to accurately mark on your body where the radiotherapy needs to be delivered
- Spinal cord – Large bundle of nerves that runs from the brain down the length of the spine
- Steroids – Medicines that help to reduce swelling around the nerves
- Urinary catheter – Small tube inserted into the bladder to help it empty. Urine collected into a bag.
- Vertebrae – Individual bones that make up the spine
Further information and advice
Macmillan/Cancerbackup www.macmillan.org.uk 0808 808 2020
Brain and Spine Foundation www.brainandspine.org.uk 0808 8081000
NICE guidance www.nice.org.uk NICE publications 0845 003 7783
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact:
……….……………………………………………………
on telephone number: …………………………
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.
