- Reference Number: HEY-460/2019
- Departments: Physiotherapy
- Last Updated: 28 February 2019
Guidance for patients and carers who have received training in the use of the Lung Volume Recruitment Bag from a qualified physiotherapist/appropriately qualified health care professional
Introduction
This leaflet has been produced to give you general information about your treatment. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your physiotherapist, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a Lung Volume Recruitment (LVR) Bag?
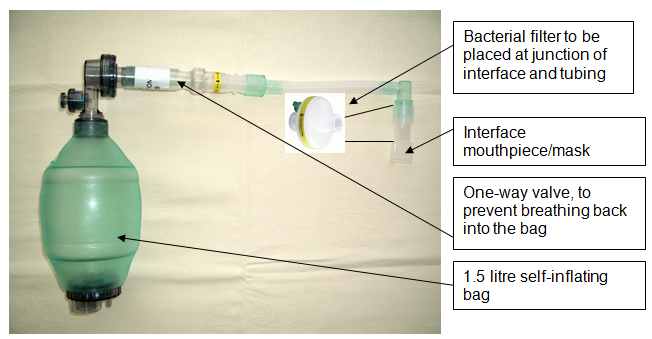
The Lung Volume Recruitment Bag (LVR) may aid you in clearing your chest secretions, also known as sputum or phlegm. The LVR bag is a 1.5 litre self-inflating bag with a one-way valve. The LVR bag can be used with either a face mask or mouthpiece.
Why do I need a Lung Volume Recruitment Bag?
The LVR bag is used to increase lung volume and aid in the clearance of chest secretions. The LVR bag is typically used with patients who have weakened respiratory muscles and/or a decreased ability to cough.
Can there be any complications or risks?
There are no recorded incidences of complications resulting from patients using the LVR bag. However, incorrect use of this device may possibly result in complications.
The primary risk is trauma or damage to the lungs as a result of over-inflation. Over-inflation is described as performing an excess of inhaled breaths that overfill the lungs and cause discomfort for the user. Trauma may result in the form of bleeding or, in a severe case; a pneumothorax (collapsed lung) may occur.
A pneumothorax occurs when the lung tissue is damaged creating a communicating hole between the lungs and the chest cavity. This allows air to build up in the chest, squeezing the lung and causing it to collapse.
There is a very low risk of this occurring, if you use the LVR bag in the way that you have been trained.
How will I be prepared for using the LVR bag?
Before you are able to use the LVR bag you and / or your carer will have been trained and observed in the use of this device by a physiotherapist or appropriately qualified health care professional. You should not use the LVR bag unless this training has taken place.
During your training you will be given every opportunity to ask questions and practice the technique in a supervised environment.
Please read this information leaflet carefully. Share the information it contains with your partner and family (if you wish) so that they can be of support to you. There may be information they need to know, especially if they are taking care of you during and following your treatment with the LVR bag.
When not to use the LVR bag
- If chest secretions are stained with blood
- Immediately after a meal (allow 1 hour after eating before using the LVR bag)
- If suffering from nausea or vomiting
- When feeling drowsy or when consciousness is impaired
- If unable to communicate via gesture or speech (e.g. blinking of the eye, raising a finger or hand)
- If you experience chest pain, chest tightness, shortness of breath or wheeze
- If you have surgery to your face, nose or mouth
- If you have surgery to your lungs, stomach oesophagus or throat
- If you have a pneumothorax (“collapsed lung”)
Seek advice from the medical team caring for you about when to start using the LVR bag if:
- You have been diagnosed with moderate to severe chronic obstructive pulmonary disease (COPD) or asthma.
- You are recovering from a heart attack or cardiac arrest/cardiac event
- You have received treatment for a pneumothorax (“collapsed lung”)
- You have been diagnosed or treated for a pleural effusion (fluid around the lung)
- You are diagnosed with bullous emphysema or lung trauma
- You are diagnosed with increased intracranial pressure or require a ventricular drain
How do I use the LVR bag?
This section should explain how to use the LVR bag as a reminder of the information you and/or your carer received during training:
- The technique is best performed in an upright sitting position (can be performed half lying 30 – 45 degrees head up, or in a position noted by the user to aid their breathing)
- Agree a communication stop – signal for when the mouthpiece/face mask is in place and the patient cannot speak e.g. hand waving or rapid blinking
- Check the pressure release valve is working on the LVR bag by blocking the face mask / mouthpiece with a clean or gloved hand to stop air escaping from the pressure release valve
- If using a mouthpiece consider the use of a nose clip, to prevent air leaking from your nose. The nose clip should be removed immediately following LVR bag use (check for skin / nasal tissue damage before and after each use)
- Ask the patient to breathe in and then place the mouthpiece in the patient’s mouth asking them to make a tight seal with their lips. If using a face mask apply to the face, covering the nose and mouth, with minimal air leaks
- Once the seal is made ask the patient to breathe in further. With each breath that the patient takes gently squeeze the LVR bag to assist. Immediately once the bag has re-inflated ask the individual to breathe in again and repeat until 3 breaths have been delivered (the breaths are stacked one after another as the LVR bag contains a one-way valve preventing the patient from breathing out)
- Once a maximum deep breath has been delivered, remove the mouthpiece and ask the patient to hold the breath for 3 to 5 seconds if this is possible
- The patient can either breathe out normally or if secretions are present they can produce a cough, which can be strengthened with manual techniques if the carer is trained in these methods
- Steps five to eight can be repeated up to 5 times in one treatment session
- If the patient starts to complain of dizziness and / or light-headedness, the treatment should stop. This is likely to have been caused by hyperventilation (over breathing)
- Allow at least 10 minutes before the next session
- If the patient complains of a sudden onset of chest pain or tightness accompanied by a sudden increase in shortness of breath, treatment should stop immediately and medical help should be sought if this does not show signs of improving within 5 minutes
- The interface (mask or mouthpiece) should be removed and cleaned under running water after each use and left to air dry
How often should I use the LVR bag?
Your physiotherapist (or appropriately qualified health care professional) will have given you instructions on how often to use the LVR bag when you were trained
You should use the LVR bag ………. per day when you do not have secretions
You should use the LVR bag ………. per day when you do have secretions e.g. during a chest infection
What happens if the LVR bag stops working?
The LVR bag can be used for up to 12 months before it will need to be replaced.
Should it become visibly contaminated with secretions in the one-way valve, or ceases to function correctly, please contact:
Community Physiotherapist/Contact………………………………….…
Telephone ………………….
If you have any problems or questions call the Physiotherapy Department on the following telephone numbers:
Castle Hill Hospital (01482) 622296 (Monday to Friday)
Hull Royal Infirmary (01482) 608764 (Monday to Friday)
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

