- Reference Number: HEY-509/2022
- Departments: Neurology and Neurosurgery
- Last Updated: 21 January 2022
Introduction
This leaflet has been produced to give you general information about lumbar puncture. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team
What is a Lumbar Puncture?
A lumbar puncture (LP) is the insertion of a small needle into your spine so that a sample of the fluid that bathes the brain and the spinal cord can be taken for testing. The fluid is called cerebrospinal fluid (CSF) and is constantly replenished; when a small sample of this fluid is taken it is rapidly replaced.
Why do I need a Lumbar Puncture?
CSF testing can provide your doctors with information about how the brain and spinal cord are working. When this is combined with a history, examination and scan results, a lumbar puncture can sometimes help to diagnose a wide range of neurological conditions. It also allows the CSF pressure to be measured to see if it is within the normal range.
Preparing for a Lumbar Puncture
Before your lumbar puncture please eat as you normally would. When you arrive for your lumbar puncture the doctor will speak to you about the procedure and answer any other questions you may have. Please make sure you empty your bladder before the procedure so that you are not uncomfortable during it. Do not drive on the day of lumbar puncture, please bring someone with you who can drive.
There is a risk of bleeding and bruising with lumbar puncture and you should tell the doctor if you are taking anticoagulants such as warfarin, dabigatran etexilate, rivaroxaban or heparin, anti-platelet drugs like Aspirin, clopidogrel and dipyridamole, or if you have a coagulopathy, abnormal bleeding or clotting disorder (bleeding disorders). Generally lumbar puncture can be performed safely if you are on aspirin but with other drugs or combinations of drugs it may be necessary to stop them temporarily. Please advise your doctor if you are taking these medications before attending for the procedure.
You may want to let your employer know you are having a lumbar puncture and that you should refrain from manual labour for a day afterwards.
What happens during a Lumbar Puncture?
The lumbar puncture takes 15 – 20 minutes. This is what happens:
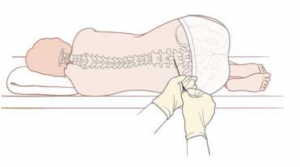
- You will either be asked to lie on your side with your knees curled up to your stomach or asked to sit on the side of the bed, bending forward. A nurse may help you tuck your head toward your chest.
- Your lower back is washed with a disinfectant to clean the skin.
- You will then be given a local anaesthetic injection to numb the area. This may sting for a few seconds.
- The doctor will carefully put a needle into a space in the lower back, below where the spinal cord ends. You will need to hold very still so that the needle does not move. You may feel some pushing as the needle enters your back, please tell your doctor if you feel pain.
- A sample of your spinal fluid is then taken and will be sent to the laboratory for testing.
- A small dressing will then be put on your back.
After your Lumbar Puncture
You will be asked to lie flat for 30 minutes after your lumbar puncture and after that you will be free to go home, unless you are being investigated for normal pressure hydrocephalus. If this is the case, you are expected to stay for a few hours to complete all the assessments.
Please drink plenty of fluids to help reduce the chance of developing a headache. If you do experience a headache after the procedure, you can treat this by lying flat and taking pain relief medication such as paracetamol. Back pain can also be treated with pain relief medication. The dressing from the lumbar puncture can be removed the following day.
Avoid strenuous activity for the first 24 hours after the procedure. You can return to all your usual activities such as work and driving, as soon as you feel well enough after that.
Follow-up Information
Some of the test results from the lumbar puncture will take a few days, but others can take several weeks. You will be advised how and when you will receive the results after the procedure and any appropriate follow-up appointments you may need. If you have any questions about this you can contact your consultant’s secretary.
What are the risks of a Lumbar Puncture?
Headache
This is the most common side effect and is due to decreased pressure of the CSF following removal of the fluid. It can start a few hours to 2 days after the procedure, and last for a few days. It is caused by the slow leak of spinal fluid through the puncture site into the tissue. It is not dangerous and the leak closes over a few days. The headache may be dull or throbbing and you may also have a stiff neck and sickness. It can be treated by lying flat and taking pain relief medication such as paracetamol.
Very rarely the headache can last several weeks or months and will need an injection to seal the lumbar puncture site. Drinking plenty of fluid and eating salted snacks can help to reduce the risk of headache. If it does not settle or is severe, let your doctor know.
Back pain
You may experience some back pain after the procedure from where the local anaesthetic injection and lumbar puncture needle was inserted, and may also have some bruising. If you have any back pain after the lumbar puncture you can treat this with pain relief medication such as paracetamol.
Tingling in your legs
Nerve damage after a lumbar puncture is extremely rare (1 in a 1000). Some times during the procedure the nerves that float in the fluid can touch the sides of the needle causing them to be stimulated, when this happens it gives a feeling of tingling down the leg that lasts for a few seconds.
Infection / fever
This is extremely rare. There is always a risk of infection being introduced, as the needle has to go through the skin. The risk is reduced by cleaning the skin and using aseptic techniques and hygiene practices. If you get symptoms of infection like a fever, you must contact your doctor immediately.
Other complications
In very rare cases a blood clot may form around the lumbar puncture site, or around the brain. This would be very serious and may require surgery to treat it. There have also been extremely rare reports of persistent back pain, numbness and tingling of the leg, hearing loss and double vision following a lumbar puncture.
Serious harm due to complications such as these occur in less than 1 in 10,000 lumbar punctures. You and your neurologist will have weighed up the risks of the procedure against the potential benefits and will always ensure that the procedure is only undertaken if it is absolutely necessary.
Symptoms to report
Please contact your doctor if you have any of the following symptoms after you have been discharged home:
- arm or leg weakness or numbness
- new incontinence or constipation
- a headache that does not resolve on lying flat
- a high temperature (38ºC or above)
- sweats
- confusion
- strong aversion to bright light
Difficulty performing the procedure
In approximately 1 in 20 patients the lumbar puncture is difficult to perform. This is more likely in people who have severe arthritis of the spine, have an abnormally shaped spine or are overweight. In these circumstances you may need another appointment to come and have the procedure performed using X-rays to guide the doctor in inserting the needle.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

