- Reference Number: HEY-385/2023
- Departments: Oncology (Cancer Services)
- Last Updated: 1 December 2023
Introduction
This leaflet has been produced to give you advice about a condition known as lymphoedema. It can be used in conjunction with the information you will already have been given by your Lymphoedema Nurse Specialist. The leaflet will help you manage your lymphoedema following your initial assessment.
Most of your questions should have been answered at your initial assessment; if, however, after reading this leaflet, you have any concerns or require further explanation, please contact your Lymphoedema Nurse Specialist.
What is Lymphoedema?
Lymphoedema is a collection of lymphatic fluid (clear fluid that circulates around the body tissues) that builds up in the tissues below the skin and causes swelling to the affected area. It will occur when the drainage routes of lymphatic fluid become blocked due to cancer or its treatments e.g. surgery, radiotherapy, tumour and trauma. Although lymphoedema cannot be cured, your individual management programme, as discussed and agreed with your Lymphoedema Nurse Specialist, can help to control and reduce your lymphoedema.
How to manage your Lymphoedema
People with lymphoedema have a high risk of developing an infection due to their impaired lymphatic system. One of the most common infections is called cellulitis, which will appear in your affected area.
The signs of cellulitis are:
- Inflammation of the skin
- Pain
- Warmth (of the skin)
- Redness of the skin (erythema)
- Flu-like symptoms such as high temperature, headaches
You will need to see your GP immediately to assess if antibiotics are required. Until symptoms have improved, it will be necessary to remove your compression garment (see below) and rest your leg. Please inform your Lymphoedema Nurse Specialist after you have seen your doctor.
Repeated attacks of cellulitis will cause further damage to the lymphatics and may result in an increase of swelling. It is important to try to reduce the risk of cellulitis by taking very good care of your skin.
You are recommended to:
- Avoid breaks in the skin.
- Use a non perfumed moisture cream to keep your skin supple and in good condition. Apply the cream daily, best done at night after your bath/shower. Apply cream in an upwards direction, starting at the top of the leg, finishing at the foot. Smooth down the hairs on the leg so that they lie naturally flat.
Management of your lymphoedema will include the following:
- Skin care
- Exercise
- Compression garment
Skin Care for patients with Lower Body Lymphoedema
The following is a list of things that will help you:
- Inspect your skin daily, looking for signs of broken areas, redness and swelling. Pay particular attention to feet and toes.
- Treat small cuts and grazes promptly by cleaning well and applying antiseptic. If the area becomes hot, red and more swollen, notify your doctor as soon as possible.
- Protect the skin on the leg from sunburn.
- Use an electric razor if and when shaving the leg.
- Dry well between the toes after a bath to prevent fungal infections such as athlete’s foot, be sure to get treatment for this if it appears.
- Take care when cutting toe nails; cuts from nail scissors may become infected. It is best to use nail clippers.
- Do not allow injections to be given in the affected leg/buttock.
- Do not take very hot baths, as this can make the swelling worse.
- Do not wear restrictive clothing, including tight underwear.
- When relaxing, elevate your legs on a foot stool.
- Avoid standing for long periods if your legs are swollen, either walk around or sit with legs elevated.
Exercises for patients with Lower Body Lymphoedema
Please ensure you are wearing your compression garment when exercising, if you have been supplied with one.
The special movements you carry out will have the following three important effects:
- Exercises will help to drain the fluid out of the swollen area. The muscles squeeze and relax as they work, which in turn helps to pump the fluid away. The pumping action is made more effective when you are wearing your compression garment as this will provide a gentle squeeze around the outside of the limb.
- Exercise will help to keep the joints moving and in good condition.
- Exercise will help to improve posture.
It is recommended that you also:
- AVOID using your limb in one position for a long time.
- AVOID over-exertion, do not strain and do not be over-vigorous.
- AVOID lifting, carrying, pushing, or pulling heavy weights.
- DO all exercises slowly.
Age and fitness will affect the amount/type of exercise you will be advised to do by your Lymphoedema Nurse Specialist.
If your mobility or balance is affected, exercises can be done whilst sitting on a chair or in bed.
f the exercises cause you pain or dizziness, discontinue until you have contacted your Lymphoedema Nurse Specialist.
If you have cellulitis you should rest your affected limb and carry out very gentle movement, e.g. bending of the knee and ankle. Try to exercise every day; swimming, walking and yoga are good forms of exercise.
Suggested exercises
Exercising your leg whilst carrying out normal day to day activities will help to manage your swelling.
Try to carry out your exercises every day.
Exercises should be gentle, keeping the joints moving and in good condition (ankle, knee and hip).
Each exercise should be repeated 5 times, increasing to 10 to 15 times, as often as you link. Please ensure you take a short break between each repetition. You can carry out your exercises as many times as you feel comfortable. Please be aware that swelling may increase if you exercise too quickly too often or for long periods without resting. If increased swelling occurs, you should stop and rest.
Illustrations provided by the Department
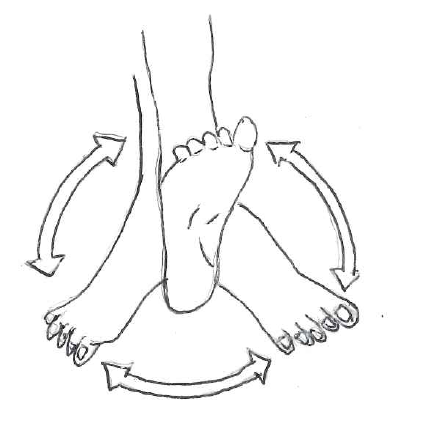
- Slowly circle your foot at the ankle.
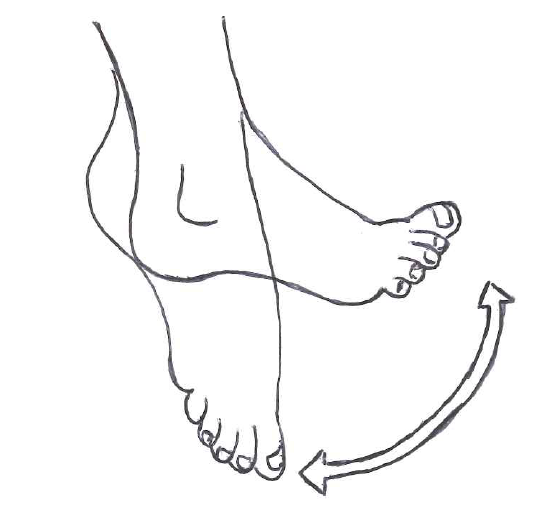
2. Slowly bend your foot at the ankle, bringing your toes towards the knee. You should feel a stretch at the back of your knee; hold for a count of five seconds and then slowly point the toes down to stretch the ankle. Hold this position for five seconds.
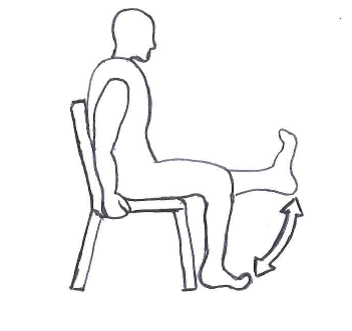
3. Either sitting on a chair or on the side of your bed, bend your knee as far as you can and then stretch your leg out straight in front of you. Try to work the muscles at the front of your thigh so that they feel firm. Hold for a count of 10 and then relax for a count of 10 before starting again.
Compression Garments
A compression garment is worn to help keep your swelling under control.
- It is best to put your garment on first thing in the morning.
- If you have any problems with applying your garment, please let your Lymphoedema Nurse Specialist know so that they can supply you with an aid for fitting and removing.
- Care should be taken not to snag or catch your garment with sharp nails or jewellery, etc.
- It must fit comfortably.
- The fabric of the garment should be gradually eased up the limb to ensure even distribution.
- Ensure there are no creases or wrinkles since this will chafe the skin and act like an elastic band, causing fluid to build up.
- The garment should not be too tight. It should feel firm and supportive but should not be painful or make the toes turn a purple/blue colour.
- Ensure the garment is not too loose or baggy, especially nearer the foot, otherwise it will not do its job.
- If the compression garment feels too long, just ease the excess material evenly down the limb.
- Never roll the tops of the garment down as this will act like an elastic band, causing fluid to build up lower down.
- All compression garments should be removed when retiring to bed at night, unless your Lymphoedema Nurse Specialist has advised otherwise.
- Skin hygiene is important.
- If you experience pins and needles, loss of sensation anywhere in the limb that you have not experienced before, an increase in pain, or if your toes turn blue, you should remove your garment immediately and inform your Lymphoedema Nurse Specialist.
- The use of rubber gloves is recommended when applying your garment as they enable you to smooth out wrinkles and grip the fabric.
- If you have an episode of cellulitis infection, please remove your garment and contact your Lymphoedema Nurse Specialist.
The care of the compression garment is to follow the manufacturer’s instructions:
- Wash the garment as per manufacturer’s instructions.
- Do not tumble dry unless advised to do so; dry away from direct heat.
- Garments should be replaced at least every 4 to 6 months as per the manufacturer’s guidelines.
The ‘Lymphoedema Support Network’ (LSN) is a patient led web site and can be used as an additional source of information www.lymphoedema.org/
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact: The Lymphoedema Team, The Queens Centre for Oncology/Haematology, Castle Hill Hospital, Castle Road, Cottingham, HU16 5JQ. Telephone: 01482461084 or 01482461110.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

