- Reference Number: HEY-782/2023
- Departments: Endoscopy
- Last Updated: 1 November 2023
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
Why do I need a Laparoscopic Nissen Fundoplication?
This operation is performed for patients with symptoms which include acid reflux or heartburn which has not completely responded to medical treatment and lifestyle adaptive changes. Patients will often have undergone tests advised by their surgeons to guide the diagnosis and help exclude other conditions, which may not respond to this surgery. These tests may or may not include endoscopy, tests of the function of the gullet (oesophageal physiology) and barium swallow X-rays.
What is a hiatus hernia?
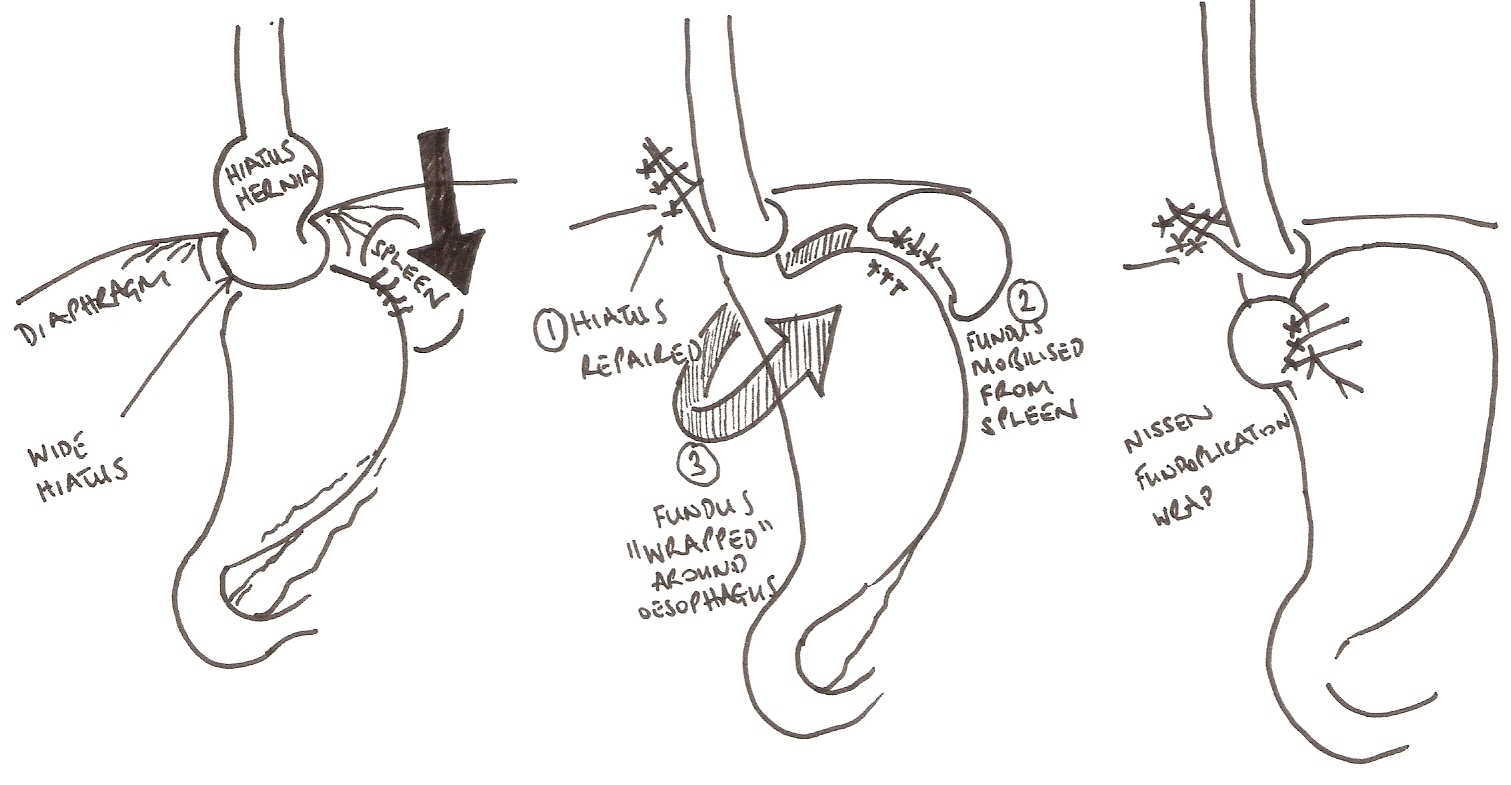
A hiatus hernia occurs when the opening in the diaphragm, which normally exists to allow the oesophagus (gullet) to pass from the chest into the abdomen (the oesophageal hiatus of the diaphragm), becomes too wide and allows the stomach to slip up into the chest. This is not uncommon and may occur in as many as 1 in 5 people.
Gastro-oesophageal reflux occurs when acid or food/fluid from the stomach leak back into the gullet causing irritation, (pain) heartburn, regurgitation or cough.
A hiatus hernia may make gastro-oesophageal reflux more likely but these two diagnoses are not the same thing. A hiatus hernia may occur without reflux and reflux may occur without a hiatus hernia. Commonly however, these two do co-exist and when surgery is needed, they are usually treated together.
Symptoms of hiatus hernia or reflux can be treated with medication (acid suppression medication, antacids) and lifestyle changes (e.g. reduction of spicy or fatty foods, alcohol, fizzy or caffeine drinks and weight reduction). An operation is an option for very carefully selected patients and is an option with its own risks.
What is a Nissen’s Fundoplication?
The vast majority of patients with a hiatus hernia and those with reflux DO NOT require surgery but in some circumstances surgery is useful and usually performed by keyhole surgery.
The operation involves two steps: the first repairs or strengthens the weakened muscle of the hiatus (opening in the diaphragm) using stitches and occasionally a reinforcement material than slowly becomes replaced by your own body’s scar tissues.
The second step involves wrapping the top part of the stomach around the lower part of the oesophagus to strengthen the valve. This might be a full “wrap” (Nissen’) or half wrap (partial fundoplication). This helps reduce reflux of stomach contents from the stomach but can also reduce the ability to belch or to vomit. If gas from the stomach cannot come up, it can be temporarily trapped in the stomach causing bloating or has to pass down and increased wind (flatus) can be a common side effect of this operation.
If you also have a hiatus hernia (when part of the stomach slides through the diaphragm into your chest) your surgeon will bring the stomach back to the original position under the diaphragm and stitch the muscle surrounding the opening to stop it slipping back up.
The operation will take between 60 and 90 minutes and is usually a keyhole operation with around 5 small incisions, usually less than 1cm in size. Very rarely a larger incision will be needed to safely perform your operation such as when there is internal scar tissue or there is difficulty with complications such as bleeding.
Complete relief of symptoms is never guaranteed and some patients may still need additional medication to control their symptoms.
Under certain circumstances surgery may need to be repeated: if the wrap has slipped or is too loose; or if the patient has persistent difficulty in swallowing.
Can there be any complications or risks?
Conversion to a conventional open operation (uncommon)
It may not be possible to complete the operation using keyhole surgery. In less than 1 in 100 cases the surgeon will need to convert to a conventional open operation using a cut in the patient’s abdomen. This cut may be 15cm to 30cm in length.
Possible complications of Laparoscopic Nissen Fundoplication and hiatus hernia repair will be discussed with you by your surgeon:
- Recurrent hiatus hernia or slippage of the wrap (uncommon)
- Injury to lung and pneumothorax (uncommon)
- Wound infection (uncommon)
- Bleeding (uncommon)
- Need for splenectomy (rare)
- Perforation and peritonitis (uncommon)
- Deep vein thrombosis and pulmonary embolism (uncommon)
- Heart attack (uncommon)
- Chest infections (uncommon)
- Death (very uncommon)
- Delayed stomach emptying (gastroparesis)
- Persistent food sticking sensation
- Late recurrent reflux symptoms (uncommon)
How do I prepare for the surgery?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
Before your operation:
You will be having a general anaesthetic and will have a pre-operative screening appointment to assess your suitability for surgery, before you are given a date for your operation. At this appointment the nurse will take details of your:
- medical history and current medication
- home care arrangements after you have been discharged from hospital including relative/friend support and transport arrangements.
Please use this opportunity to ask any questions about your surgery and aftercare. You will also be given instructions about preparing for your operation, which will include advice about:
- having a bath or shower before you come to the hospital
- eating and drinking
- pausing or taking your normal medication, if appropriate
- returning to work after surgery
On the day of admission please bring:
- this information leaflet
- all medication in original containers along with the electronic printed list supplied by your doctor if available
- dressing gown, slippers and small overnight bag/toiletries in case of overnight stay
- contact telephone number for a lift home
- something to read or to occupy you to pass the time
Please do not:
- bring any valuables or wear jewellery
- wear nail varnish or false nails
- wear face make up or lipstick
What will happen?
On the day of surgery
You should have a bath or shower before you come to hospital. Do not eat from 2.00am, however you are encouraged to drink clear fluids only up to 6.00am, e.g.no milk or pure orange (black tea or coffee is allowed). Chewing gum is not allowed on the day of surgery. If you wear contact lenses, you will need to remove them prior to your operation. Please bring your spectacles or an extra pair of contact lenses with you.
On admission to the ward you will be greeted by a nurse who will check that your details are correct. The surgeon and the anaesthetist will talk to you and you will be invited to ask any questions you may have before signing your consent form. You will also be given compression stockings to wear.
A member of staff will escort you to the operating theatre. After the operation, you will recover in a special recovery area near to theatre until you are awake sufficiently to return to the ward.
What happens afterwards?
Following your operation
After the operation, you will recover in a special recovery area near to theatre until you are awake sufficiently to return to the ward. You will then be transferred to the ward area where nurses will continue to monitor your condition.
Initially you may also have some neck and shoulder tip pain, this is due to the gas used (carbon dioxide) to enable a clear view inside your stomach, which can get trapped. It will disappear by itself after a couple of days. If you feel any discomfort, please inform the nurse looking after you, so that pain relief can be given. If you feel sick after the operation you will be given medication for this and remain nil by mouth until the nausea and sickness wears off. Your anti-reflux medication should stop at the time of the operation.
After a few hours you may be allowed to take sips of fluids only. If you are able to tolerate sips you may then be able to build up to free fluids. On the first day after your surgery you can have a liquid diet.
If the doctor feels you are sufficiently recovered you will be discharged home. Sometimes patients may go home on the same day as their operation although most patients stay in one night. It is important that you arrange someone to collect you at an appropriate time, if you have stayed overnight, this will be before 11.00 am. Due to the nature of the ward you may be expected to vacate your bed early and wait for your discharge transport in a discharge area.
Before discharge you will receive a dietary advice leaflet. It is important to follow dietary advice to prevent a blockage, discomfort and vomiting. Your stomach may have reduced in size slightly; therefore you may feel full easily. We recommend you eat little and often.
It is advisable to avoid bread and fizzy drinks for the first 4 to 6 weeks. You will notice during the first few weeks that food tends to stick, therefore it is important to eat slowly and to chew food thoroughly. It often helps if you drink fluids with your meal.
Care at home
You will have some mild pain for up to a week after the operation. You will be prescribed pain relief medication to take home with you. Please take only as directed. You will need to continue to wear the compression stockings on your legs that were applied prior to the operation for 5 days (day and night).
You should seek medical attention immediately if you develop:
- severe abdominal or chest pain
- vomiting and cannot keep fluids down
- severe difficulty in swallowing where food becomes stuck
You will be informed if the stitches in your wound are dissolvable or need to be removed. Some patients have Steri-strips (small strips of adhesive tape) rather than stitches in their wounds. Even if you have dissolvable stitches, it is recommended that you have your wound checked by the Practice Nurse at your GP surgery 4 to 5 days after your operation. You may shower on the day following your surgery. Any waterproof dressings over your wounds should remain in place for 5 days and then you may remove them.
You should remain off work for approximately 2 weeks, or as directed by the surgeon. Your surgical team will provide initial fitness for work certificates and any required extension is provided by your doctor. You will be followed up in clinic by your surgeon.
Driving and Flying
You should not drive until you can perform and emergency stop but please clarify this with your insurance company. This will not be for the first 48 hours following your surgery. Please check that your insurance policy does not prohibit you from driving for a longer period, following general anaesthetic or surgery. Based on Civil Aviation Authority guidance we recommend at least 48 hours before flying after keyhole surgery or 10 days after an open surgical operation.
If you experience problems regarding your surgery after being discharged
PLEASE ALWAYS CALL FIRST FOR ADVICE
It is important you DO NOT present yourself to the ward from where you were discharged. Telephone the ward from which you were discharged – Monday to Friday 8.00 am – 6.00pm. After 6pm and weekends – contact Ward 14 Castle Hill (01482) 623014.
If you are unable to get in touch with Ward 14 please call your doctor’s emergency service or 111.
You will receive advice over the telephone as to the appropriate care for you. This may be:
- over the telephone advice
- to contact your doctor’s practice to arrange a nurse-led clinic appointment
- an urgent outpatient clinic follow up appointment with your surgeon
- to contact your doctor to arrange emergency admission to Hull Royal Infirmary
If you are severely unwell contact your emergency doctor or Hull Royal Infirmary Emergency Department. Castle Hill Hospital does not have on site emergency services.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

