- Reference Number: HEY-430/2016
- Departments: Orthopaedics
- Last Updated: 1 June 2016
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should be answered by this leaflet/booklet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
What is an arthroscopy?
An arthroscopy is a “key-hole” operation which is used to look inside of joints and is especially common with the knee joint. This is performed using a series of very small cuts in the skin, to make two or three small portals (holes) within the knee joint.
- The arthroscope (camera) is inserted into one of the portals.
- A second portal can be used to flow a saline solution through the knee joint, which improves visibility and manoeuvrability of the instruments.
- The third portal is for the arthroscopic instruments.
An arthroscopy allows the orthopaedic surgeon to examine the knee joint, which allows an accurate diagnosis and treatment to be carried out. Each arthroscopy operation is different and the treatment will depend upon what the arthroscope shows once inside the knee joint. This operation may be done either under a local anaesthetic (whilst you are awake) or a general anaesthetic (whilst you are asleep).
Why do I need an arthroscopy?
An arthroscopy is extremely useful in confirming the cause of knee symptoms, and then delivering the appropriate treatment. This may be extremely beneficial if you are experiencing any of the symptoms detailed below:
- Pain in the knee joint
- Intermittent swelling at the knee joint
- Giving way
- Locking of the knee joint
Some of the operations, which can be performed at the knee using an arthroscopic approach include:
- Trimming or repairs of specialised knee cartilage (meniscus)
- Removal of loose bodies (cartilage/bone)
- Micro-fracture treatment for osteochondral defects (bone-cartilage defects)
- Reconstruction of ligaments
- Trimming of other soft tissues (ligaments, plica, and bursa)
- Release of soft tissue to correct patella tracking problems
Can there be an complications or risks?
As with any surgery there are risks involved. The consultant will inform you of these risks prior to your operation. These risks include:
- Bruising and swelling
- Infection
- No change or recurrence of symptoms
- Stiffness in the knee
- Unexpected reaction to the anaesthetic
- Damage to nerves and blood vessels possibly requiring further surgery
- Loss of feeling around the operation wounds
- Blood clots in legs and/or lungs, stroke, heart attack or heart failure, all which can result in death
- Complex regional pain syndrome which is an uncommon form of chronic pain. The pain usually develops after an injury which in most cases is a minor injury or surgery but the pain experienced is out of all proportion to what you would normally expect.
What happens afterwards?
Post-operative advice
- You should refrain from the consumption of alcohol or taking any medication other than that prescribed by the nursing staff (including sleeping tablets) for 48 hours.
- When you feel ready, you may eat and drink.
- You may return home once in a stable condition and the nursing staff have arranged your discharge medication and information.
- If you have had a general anaesthetic, we also advise you not to operate machinery or household appliances. We also advise that you have somebody drive you home and stay with you for the first 24 hours following the operation.
What to look out for
If you experience any of these symptoms following the operation you must contact the hospital immediately.
- Fever
- Cold sweats/chills
- Persistent warmth or increased redness around the knee joint
- Increased pain around the knee joint without a change in medication (pain relief)
- A significant increase in the amount of swelling at the knee joint
- A pain in the calf muscle with associated swelling and redness
Follow up with the consultant
Following the arthroscopy you may be visited by the consultant on the ward/day surgery unit for further assessment and to discuss the operation. A follow-up appointment will be sent out in the post, asking you to attend the outpatients department. This will be arranged for approximately 2 weeks following the operation.
Driving
You should refrain from driving for at least 2 weeks following your surgery. You should also contact your insurance company to notify them about your operation and to check the validity of your insurance. You should then seek further advice from your consultant and your insurance company as to when you can start driving again. Upon the follow up assessment the consultant may state that there is no medical reason to stop you from driving again. However this essentially will be your own decision as to whether you are safe to drive and can perform all the essential driving manoeuvres.
Wound care
Please keep all dressings clean and dry for two days following the operation. After two days you may remove the bandages, but leave the adhesive dressings on until you are further reviewed in the outpatient clinic, which is usually within two weeks following the operation.
Returning to work
This will depend upon the specific details of your operation and also the nature of your work. Usually at least one week off work is required, however this may need to be longer if your work is specifically manual/physical. This should be discussed with your consultant for further advice on this matter.
Return to exercise and sport
This will depend upon the specific details of your operation. This is something that should be discussed with the consultant or your physiotherapist.
Post-operative exercises
There are a wide range of exercises detailed within this leaflet, but these may be modified by the physiotherapist according to your specific operation.
Swelling control
It is generally advised that you elevate the leg on a regular basis for the first 48 hours after for operation. This will reduce the risk of swelling and pain.
As long as there is no reduced sensation at the operation site then an ice pack may be applied to the knee joint to reduce swelling also.
- Cover your knee with a damp tea-towel or cloth. It is important that ice is not applied directly onto the skins surface as this can cause an ice burn.
- Use either ice in a polythene bag (ice pack) or a pack of frozen peas.
- Place the ice pack over your knee, holding this in place with a towel.
- Leave the ice pack on for approximately 10-15 minutes, inspecting the skin on a regular basis.
- It is normal for the skin to become cold and slightly red. If there is a significant increase in pain then remove the ice pack immediately.
Walking normally
Generally you are allowed to walk full weight-bearing or as pain allows after the operation. If this is restricted to either non-weight bearing or partial weight bearing then this will be assessed prior to your discharge.
It is important to try and walk normally.
- The first part of the foot to make contact with the floor should be the heel and last part of the foot to leave the floor should be the big toe as you push off.
- Try and place one foot in front of the other as you walk.
- Try and bend the operated knee as it swings through.
Stairs
When going up the stairs, it is easier to lead with the unoperated leg taking one step at a time.
When coming down the stairs, it is easier to lead with the operated leg, again taking one step at a time.
Remember – good leg up first – operated leg down first
Breathing exercises
To prevent chest complications it is advised that you perform 10 deep breaths and 2 – 3 coughs every hour to keep the chest clear from infection. If you suffer with chest problems, the physiotherapist may show you some specific exercises.
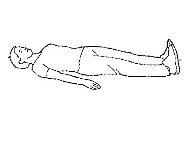
Circulation exercises
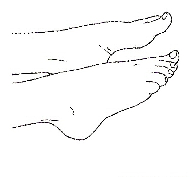 |
|
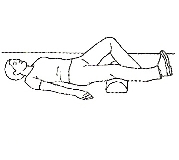
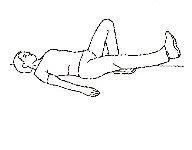
Movement of the knee
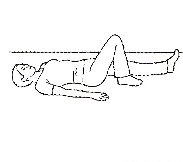 |
|
 |
|
Movement of the knee cap
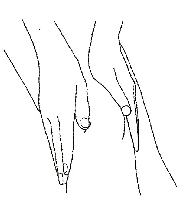 |
|
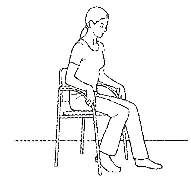
Strengthening exercises
 |
|
 |
|
 |
|
 |
|
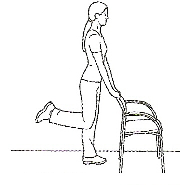 |
|
Images ©PhysioTools Ltd.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the hospital switchboard (01482) 328541 Hull Royal Infirmary or (01482) 875875 Castle Hill Hospital.
Hull Royal Infirmary:
Ward 12: (01482) 675012.
Day Surgery: (01482) 675066.
Castle Hill Hospital:
Ward 9: (01482) 623009.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

