- Reference Number: HEY-036/2021
- Departments: Oncology (Cancer Services), Radiotherapy
- Last Updated: 31 July 2021
Introduction
This leaflet has been produced to give you general information in relation to your treatment. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is Brachytherapy?
Brachytherapy is a form of radiotherapy where a radioactive source is stored and delivered via a treatment machine called a Flexitron. The radioactive source is placed close to the tumour through the use of hollow intra uterine applicators. The purpose of this technique is to deliver a direct dose to the area concerned while minimising the dose to the normal surrounding tissue. The radioactive source is stored in the machine and is moved into position to deliver the treatment.
What will happen?
Once you have completed your external beam radiotherapy your Brachytherapy treatment will not commence immediately. You will need to be booked into the next available theatre session. The Brachytherapy Team will provide any additional information you may need prior to your procedure.
Whilst undergoing your external beam treatment we will arrange for you to see the ward staff to organise your admission and pre assessment for the Brachytherapy procedure.
The Brachytherapy procedure requires you to undergo a general anaesthetic to allow the applicators to be inserted. The day before the procedure you will be admitted to Ward 30 at the Queen’s Centre, Castle Hill Hospital. We would advise you to bring an overnight bag and any medication that you are currently taking. Prior to your treatment we would also advise you follow a low residual diet (this will have already been explained to you prior to being given this leaflet). You should not eat or drink after midnight on the night before the procedure. Intra-Uterine Brachytherapy treatment is often in 3 treatments.
These treatments will take place over 2 consecutive weeks, an example of this can be found in the table below.
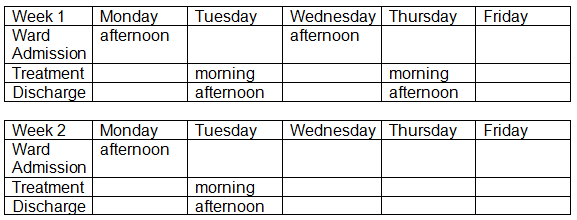
You will be admitted onto the ward the day before to your Brachytherapy treatment.
On the morning of your treatment you will be taken to the theatre at approximately 07.30am to prepare you for your anaesthetic. Once you have been anaesthetised the doctor will examine you and insert the applicators.
As the applicators have to stay in place until each individual treatment is completed, a catheter will be placed in your into your bladder to enable you to pass urine during this time. The applicators will be kept in position with gauze packing; you will be able to feel the applicators between your legs.
The applicators will be connected via a small hollow flexible tube to the afterloader. A radioactive source will travel down the hollow tube via a thin wire and will stop at programmed points to deliver your treatment. The afterloader will be switched on once the Therapeutic Radiographers have left the room and have closed the door. The Radiographers will communicate with you over the intercom and will monitor you via CCTV. When the treatment is complete the Radiographers will enter the room to remove the applicators and gauze packing.

(Photo: An example of the afterloader treatment unit and couch used for this procedure)
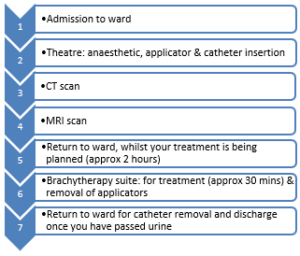
An example of a daily Brachytherapy treatment pathway
After each treatment you must not drive yourself home as you may feel sleepy for up to 24 hours. If you have any transport queries check with the ward staff.
What happens afterwards?
Therapeutic radiographers will again go through the potential side affects you may experience after treatment. You can contact us on the phone numbers provided if you have any concerns or experience any significant side effects after treatment. You will see your Doctor approximately 6 weeks after your treatment is complete.
Are there any side effects to the treatment?
Acute Side Effects: It is quite normal to experience slight bleeding, abdominal cramps and vaginal discharge after the treatment.
Mild Side Effects: May include diarrhoea and a burning sensation when passing urine (cystitis). If you have already experienced these side effects from your external beam radiotherapy; this treatment should not make them any worse. Side effects can continue for up to 2 weeks after your treatment is complete. To minimise the side effects, it is suggested that you drink plenty of fluids. If the side effects persist please do not hesitate to contact the Brachytherapy Team, your Gynaecological Nurse Specialist or your doctor.
Late side effects: The treatment can cause inflammation of the vagina and dryness. The vaginal walls can lose elasticity which can lead to the narrowing of the vagina and this can make sexual intercourse and internal examinations difficult or uncomfortable. To help prevent this, vaginal dilators and/or regular gentle sexual intercourse is recommended. The Brachytherapy Radiographers will discuss this with you and will answer any questions or concerns you may have.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact a member of the Brachytherapy Team who can be contacted via Radiotherapy Reception or the Brachytherapy Suite.
Radiotherapy Booking Office (01482) 461187 / 461188 / 461189
Radiotherapy Reception (01482) 461191
Brachytherapy Suite (01482) 461950 / 461951
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
RESEARCH
The Trust is research-active with a research strategy that includes cancer treatment and care. The radiotherapy department participates in national and international research studies to improve treatments to make them safer, more effective and to reduce side effects. We also develop patient-centered local research to improve your radiotherapy experience to benefit you and your family. We would like to encourage you to feedback about your experiences and ideas to help us to research the areas that are important to you. Your treatment will not be affected in any way should you not wish to take part.
RADIOTHERAPY STAFF
CLINICAL ONCOLOGIST, REGISTRAR, CONSULTANT THERAPEUTIC RADIOGRPHERS
They are experts in radiotherapy and will be managing your treatment. They will take the responsibility for deciding what dose and how many treatments will be best for you; they will oversee the planning of your treatment. You may see them or a member of their team at your initial planning appointment and you can see them during your treatment if you have any problems or queries.
THERAPEUTIC RADIOGRAPHERS
Radiotherapy is delivered by male and female therapeutic radiographers who are specialist healthcare professionals that are trained to plan and deliver radiotherapy treatment and to use the specialist equipment. You will usually see the same team of radiographers and they will assist you with any questions or problems or refer you to a more appropriate person.
RADIOTHERAPY SUPPORT TEAM
The team consists of Nurse Practitioners, Registered Nurses, Radiographers and Clinical Support Workers (CSW’s), who are based within the Radiotherapy Department where they actively support and advise patients receiving radiotherapy treatment. They offer advice to patients and their families/carers and are able to make appropriate referrals and
PHYSICISTS, PLANNING DOSIMETRISTS AND MACHINE TECHNICIANS
Medical physicists are specialist healthcare scientists who have a key role in the individual planning of your treatment, along with the planning technicians. They may also have an input into the set-up of your treatment. They work together with the machine technicians to ensure that the machines are reliable and working accurately.
STUDENTS
At some point during your treatment you may encounter student radiographers. Everything they do is supervised fully. If you would prefer our students not to be present during the planning and treatment, please let a member of staff know when you attend for your initial planning appointment.
OTHER MEMBERS OF STAFF
During your treatment course you may meet our receptionists, dieticians, oncology health staff, patient services staff, porters, volunteer workers. All are working together to provide you with a high quality of healthcare.
USEFUL CONTACTS
Cancer Psychological Service
Can help with achieving the best possible quality of life during and after your journey with cancer. Offer emotional support and practical help. Discuss any matters that are concerning you and your family. For a call back from the drop-in team call 01482 461060 / 461061 Monday- Friday between 9.00am and 3.00pm
Macmillan Cancer Support
Provide information from specialist nurses on all aspects of cancer and its treatment, and on the practical and emotional aspects of living with cancer. You can drop into the Macmillan Cancer Information Centre at the Queen’s Centre or call them on (01482) 461154 Monday – Friday 9.00am – 5.00pm.
Alternatively, free phone the national help line: 0808 808 0000 Monday – Friday 9.00am – 8.00pm. Online: http://www.macmillan.org.uk
Write to Macmillan Cancer Support, 89 Albert Embankment, London, SE1 7UQ
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

