- Reference Number: HEY1242/2021
- Departments: Radiology
- Last Updated: 30 June 2021
Introduction
This leaflet has been produced to give you general information about having insertion of a tunnelled central venous line (central line). Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a central line?
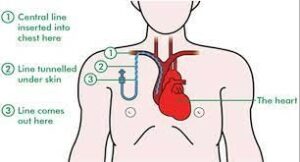
A central line is a long thin and hollow plastic tube called a ‘catheter’ or ‘line’ which is placed in a vein and this provides a way of giving you regular intravenous (IV) medication. This means you do not need to have a needle inserted every time you have treatment.
The long catheter is placed into a vein in the neck or front of the chest. The catheter extends from its entry point into a ‘central vein’ next to the heart. The larger central vein can tolerate the catheter line much better than a small vein. The catheter can stay there safely for weeks or months, sometimes more than a year. The line will be ‘tunnelled’ under the skin to reduce the risk of infection and help it remain secure.
 With kind permissions of Macmillan Cancer Support
With kind permissions of Macmillan Cancer Support
Why do I need a central line?
Intravenous medicines are given through a vein. If the IV medicine is needed short-term whilst you are in hospital then a standard IV drip into a small vein in the arm will be adequate.
However, some IV medications are required over a longer period of time. While standard IV drips work well for short-term treatment, they cannot be used for more than a few days. One way of delivering long term IV medication is via a central line.
You may need a central line for one of the following:
- Long term antibiotic treatment
- Chemotherapy treatment
- Liquid food if you are unable to eat
- Haemodialysis – a treatment for patients whose kidneys do not work properly
Can there be any complications or risks?
Complications are very uncommon. The central veins are near to other structures so there is a small (1%) possibility of puncturing either a neighbouring artery, or a lung (pneumothorax).
Although the procedure is carried out using a sterile technique, there is a very small risk of infection during insertion. However, there is the possibility that the tunnel where a line sits may become infected later, so great care must be taken to keep the line insertions site clean, dry and covered. It must only be used by a suitably trained person.
There is a small risk that the line may become dislodged before it is fully embedded. Care must be taken not to pull the line, especially for the first 2 weeks.
How do I prepare for the central line insertion?
Please read this information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this procedure.
The procedure is carried out under local anaesthetic in the Radiology Department. There are no specific preparations that you need to make and you may eat and drink normally prior to the procedure.
You will need to alert the staff of any allergies you have, and they will need to know a list of your current regular medication. Please inform the staff if you take any medication to thin your blood as this may need to be omitted for a day or two prior to your procedure.
What will happen?
The procedure will be performed in the Radiology Department at either Hull Royal Infirmary or Castle Hill Hospital. This is similar to an operating theatre where special X-ray and ultrasound equipment is available.
You will have preliminary checks made by a radiology nurse such as blood pressure reading and arrangements for who to contact to take you home.
You will meet the Interventional Radiologist who is a doctor with special expertise in reading X-rays and using these to guide catheters and wires to aid treatment. The radiologist will explain the procedure and ask you to sign a consent form. This is to ensure you understand the test and its implications. Please feel free to ask any questions that you may have and remember that, even at this stage, you may decide against going ahead with the procedure if you so wish.
You will be asked to change into a hospital gown. You will lie on your back on the X-ray table and you will be attached to a monitor to check your blood pressure and oxygen levels.
The skin around the neck will be cleaned with antiseptic (this can sometimes feel cold but will not be painful). The upper half of your body, your head and part of your face will be covered by sterile sheets. The radiologist will inject some local anaesthetic into the neck to make it numb. The radiologist will then make a small nick in the skin. A needle is then inserted into the vein. A fine plastic tube called a catheter is then placed over the wire and into the vein. The radiologist will watch all of this on a tv-like monitor. A special clear X-ray dye called contrast, is then injected through the catheter. This dye allows the blood vessels to be visible on the X- ray and will help the doctor guide the placement of the central line. You will be asked to hold your breath while some of the X-rays are taken. You will feel some pushing as the line is ‘tunnelled’ through the skin. If you wish, you may be able to see the X-ray pictures on the screen after the test. When the radiologist has placed the line, it will be sutured (stitched) into position and a sterile dressing applied. There may be a small amount of oozing around the entry site, but the nurses will keep a close eye on this for you.
Is it painful?
When the local anaesthetic is injected into the skin you may feel some discomfort like a bee sting. After this, the procedure should not be painful but you will feel an uncomfortable pushing sensation when the line is tunnelled. There will be a nurse standing nearby looking after you during the procedure. If the procedure becomes painful, please inform the nurse or doctor so that they will be able to give you some pain relief medication.
What happens afterwards?
You will be taken out of the X-ray theatre into a recovery area. The nurses will carry out regular observations such as pulse and blood pressure measurements, to ensure that there are no problems after the procedure. They will also look at the skin entry site in your neck. You will have to stay in the department for a period of observation after the procedure.
You will be allowed to go home on the same day, unless you are already an inpatient. You should not drive immediately afterwards, you should arrange for someone to take you home. You may resume normal activity the following day.
The doctors who referred you for your line will then take over your care. You will have weekly appointments for the line to be checked and flushed, to prevent it from blocking. The caps on the end of the line and the dressing will be changed weekly.
It is safe to bath and shower with the line in. You will need to put the external part into a plastic bag and tape it to your skin to keep it dry. Strenuous gym exercise and sports such as golf and tennis should be avoided to prevent the line becoming dislodged, but discuss this with your doctor if you are unsure.
It is possible for a line to become infected. Please contact the team looking after you if you notice any of the following:
- Pain, swelling or redness or discoloured fluid at the insertion site
- A high temperature
It may be helpful to make a note of your care team contact number here:
………………………………………………………………………………………
Will the central line stay in?
Some lines remain in place for up to a year following placement, depending on why the line was needed. Your doctors will advise the best course for you, and a further appointment will be given to you for removal of the line.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to Interventional Radiology Department (01482) 675667 (HRI) and (01482) 622042 (CHH)
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

