- Reference Number: HEY-107/2023
- Departments: Maternity Services
- Last Updated: 12 June 2023
Introduction
This leaflet has been produced to give you general information about the procedure of induction of labour. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your midwife or doctor but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with the midwife or doctor.
There is also a video on the Maternity service website that gives you a ‘virtual tour’ of the clinic and what we do: https://www.hey.nhs.uk/maternity/induction-of-labour-clinic/
| PLEASE BE AWARE THAT INDUCTION OF LABOUR CAN TAKE A LONG TIME; POTENTIALLY 10 DAYS. IT IS IMPORTANT TO CONSIDER THIS WHEN TAKING LEAVE FROM WORK |
What is induction of Labour?
In order for a baby to be born the cervix (the neck or opening to the womb) has to change from being closed, long and hard (touching the end of your nose, is similar to feeling the cervix) to being short, soft and starting to open. When that change happens, the strong ‘working’ contractions of labour start. Your womb has a powerful muscular wall that tightens and then relaxes; these contractions gradually open your cervix. In most pregnancies this starts naturally between 37 – 42 weeks and is called ‘spontaneous labour’.
Induction of labour is a process that tries to start labour artificially by opening and softening the cervix enough to break the waters around the baby. The final stage of the process is breaking the water around the baby and, if necessary, using a hormone ‘drip’ to start contractions.
When might I be offered induction of labour?
There are three main reasons why induction of labour (IOL) is offered:
- Prolonged pregnancy – pregnancy that continues after 41 weeks.
After 41 weeks there is a slight increase in the risk of your baby developing health problems. We therefore recommend Induction of labour between 41 and 42 weeks. - Pre-labour rupture of membranes – (the waters around the baby breaking) if spontaneous labour does not happen approximately 24 hours after the waters break there is a small risk of infection to the mother and / or the baby.
- Medical reasons – If it is felt that your health or your baby’s health is at increased risk if the pregnancy continues.
Can I choose not to be induced?
After considering all the facts around IOL, if you decide you do not want to be induced, you should tell your midwife. You can be offered an appointment to attend hospital so we can check that you and your baby are well. There will be an opportunity to discuss with a midwife or doctor why you do not want to be induced and a plan will be put into place to support your decision.
It is usually recommended that we keep a closer eye on you and your baby in these circumstances. How often you come to the hospital for checks depends on your situation. The midwife or doctor will discuss this with you.
Membrane Sweep (stretch and sweep)
Once you have reached your due date, you will be offered a membrane sweep at around 40 weeks, which may be followed by another at 41 weeks. This procedure has been shown to increase the chances of labour starting naturally within 48 hours of the procedure and can reduce the need for other methods of induction of labour.
You will also be offered a membrane sweep if induction of labour is being done for medical reasons. The timing will be advised by the doctor responsible for your care.
A stretch and sweep is a vaginal examination that can be carried out at home or at an Antenatal Clinic. The procedure involves the doctor or midwife putting two fingers inside your cervix and making a circular sweeping movement to separate the membranes from the cervix. This increases the production of hormones called prostaglandins which can encourage labour to start.
There may be some discomfort or bleeding but it will not cause any harm to you or your baby. It will not increase the chance of you or your baby getting an infection.
Sometimes the cervix is not ready to have a membrane sweep performed. This is not a problem, it simply means the body has not started to produce the hormones and chemicals needed to change the cervix at the time the membrane sweep was attempted.
Where will labour be induced?
The majority of women will be managed in an outpatient setting. All women come to an Induction of Labour Clinic to have the procedure started.
Most women will be able to go home afterwards, but sometimes you will have to stay in hospital because of medical reasons or the method of induction being used. You may want to pack a birth bag and either bring it with you or have it available in your car. Please DO NOT bring a car seat with you. It is unlikely that baby will be born on the day your induction is started.
If your cervix is already favourable to have the waters around your baby broken when you come to clinic, or if the waters have already broken you will be placed on the waiting list to be induced on the Labour Ward.
Please be aware that artificially breaking the water around the baby can only be done on Labour Ward.
Admission to the Labour Ward will be managed according to individual needs and this may happen straight away or more likely you will be asked to wait at home until you are called to attend Labour Ward.
It is very important that we have the correct contact details for you and you keep your phone switched on all the time as you can be called to Labour Ward at any time day or night.
While you are waiting at home you will be asked to come into the Induction of Labour Clinic to monitor you and your baby. How often depends upon why you are being induced.
An outpatient induction of labour:
- Reduces the amount of time you will need to stay in hospital before your labour begins.
- Allows you to stay at home which evidence has shown helps labour to progress as you are in a familiar place.
- Makes the process of induction as close as possible to going into labour naturally
Your midwife or doctor will assess if you are suitable for outpatient induction of labour and discuss this with you.
At very busy times, the start of the induction process may be delayed. Very rarely it may be delayed for over 48 hours. If you are at home, you may be advised to come in to the Induction Clinic to have an antenatal review and to monitor your baby with a cardiotocograph (CTG) machine. You will be able to go home afterwards if there are no concerns about you or your baby.
What will happen?
When you come to clinic the midwife will introduce themselves and discuss everything with you to make sure you understand the procedure. Please feel free to ask any questions or voice any concerns or anxieties. We understand that Induction of Labour can make you feel anxious and scared and it is sometimes difficult to remember any questions or things you want to say so it might be useful to write down anything you want to discuss. We are here to listen to you and help if we can..
When you arrive, the midwife will do a full antenatal check on you and your baby. Your baby’s heartbeat will be monitored using a cardiotograph (CTG) machine that gives a paper recording of the heartbeat.
You will have a vaginal examination to determine if your cervix is ready to be able to break your waters (Artificial Rupture of Membranes/ ARM). In order to break the waters your cervix needs to have changed from being long, closed and hard to being thin, soft and stretchy and starting to dilate (open up). This naturally happens at the end of the pregnancy when the body starts to produce the hormones that start labour but it might not have started to happen if labour is induced before your due date.
Methods used to prepare the cervix
These are used to soften and open the cervix in order to be able to ‘break the waters’ around the baby. They may sometimes cause contractions to start as well.
You may need just one or all of these methods.
Cervical Ripening Balloon Catheter
The balloon catheter is the only method used for outpatient induction of labour. This is because it has minimal side effects and does not need you to be monitored as closely as when using a medical method.
The procedure involves a catheter (a soft silicone tube) being inserted into your cervix. It has a balloon near the tip and when it is in place the balloon is filled with a sterile saline (salt water) fluid. The catheter stays in place for 24 hours, with the balloon putting gentle pressure on your cervix. The pressure should soften and open your cervix enough to be able to break the waters around your baby or it may start labour. It is important to realise that this does not happen for everyone and you may need to progress to other methods.
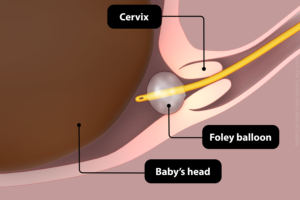
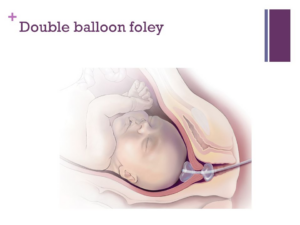
Sometimes a double balloon is used especially if your cervix is very long or hard. It works the same as a single balloon
The balloon catheter may fall out by itself or will be removed by a midwife the following day.
Going home after cervical ripening balloon catheter
During the time you are at home, you can do things as you would normally, for example, showering, bathing or walking. However, please avoid intercourse. After going to the toilet please wash your hands, make sure the catheter is clean and change underwear regularly.
If you have any of the following:
- Bleeding enough to soak through a sanitary towel
- Contractions
- Concerns about the baby’s movements
Or
- You feel unwell
- The waters around the baby break.
- The balloon falls out
You are advised to call Maple Ward on (01482) 607779. A midwife will talk with you and advise you what you need to do.
Prostaglandin
Prostaglandin is a hormone that is naturally produced by the body. It is involved in starting labour. We use two methods to deliver an artificial version of prostaglandin.
- A pessary known as ‘Propess’® is inserted into the vagina and place behind the cervix. It has tape attached so it can be removed easily. It releases the hormone slowly over 24 hours but will be removed earlier if labour starts or there are any concerns about you or your baby’s health.
- A tablet called ‘Prostin’® is inserted into the vagina and next to the cervix. You will be re-examined six hours after the first tablet; if the cervix is still not ready for the waters to be broken or you have not started in labour then a second Prostin® tablet will be inserted into the vagina.
You will have to stay in hospital if these methods are used, as your baby will need to be monitored every eight hours. Between monitoring, you will be encouraged to walk about or use the ‘birthing balls’, as being active can help to encourage labour to start.
It is important to be aware that the process of softening and opening the cervix can take up to three days if you are over 41 weeks and up to five days if we are inducing you earlier than 41 weeks. It is also important to know that it may fail completely.
You may become favourable to have your waters broken (ARM) at any point during the process. When that happens the Induction process has worked and you will be placed on a waiting list to go to the labour ward to have your waters broken.
You may become favourable for ARM, the waters may break by themselves, or you may go into labour at any point in this process.
Previous Caesarean Section
If you have had a previous Caesarean Section, you will only be offered the balloon catheter as a means of inducing labour. You may be offered another balloon catheter if the first one is not successful. You will not be offered prostaglandin as it increases the chance of the scar separating or tearing.
What happens next
When the cervix is favourable to have the waters around the baby broken, known as an Artificial Rupture of Membranes (ARM), you may be able to go home and wait to be contacted by the Labour Ward with a time for admission.
THIS CAN TAKE UP TO FIVE DAYS. The consultant in charge of the Labour Ward will make a decision about when to admit you to the Labour Ward based on medical needs and at all times keeping in mind the safety of your baby and you. If you are being induced because you are Post-dates (over 41 weeks) you will be a priority to go to Labour ward.
If you are being induced as an outpatient, this will NOT affect the decision about when you will be admitted to the Labour Ward.
During this ‘waiting time’ you will be offered appointments in the Induction Clinic so we can monitor your baby and yourself and give membrane sweeps if you want. How often this happens will depend on the reason why you are being induced.
If your waters break by themselves then you may be able to wait to see if you go into labour. If you do not, then labour will be induced with the hormone drip approximately 24 hours following the waters’ breaking.
If you go into labour by yourself, you are no longer on a ‘waiting list’ but will be admitted to the Labour Ward or Midwifery -Led Unit when labour is established.
If the process has failed you will be offered a planned Caesarean Section. Your Consultant and the ward staff will arrange all this for you.
What happens on the Labour Ward
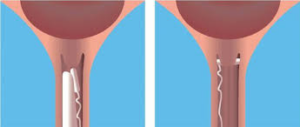
Artificial rupture of the membranes (ARM)
When the cervix is soft, open to around two to three centimeters and the baby’s head has gone down into your pelvis, it should be possible to ‘break the waters’ around the baby.
This procedure is carried out by using a small plastic hook which releases the water and allows the pressure of the baby’s head to press on the cervix and stimulate contractions. It will not harm you or your baby. The procedure may be uncomfortable but it should not be painful.
You may be given some time to see if contractions start or we may use an artificial hormone called Syntocinon® straight away.
Oxytocin (Syntocinon®)
This is an artificial form of the hormone that causes your uterus (womb) to start having contractions.
It is given through a tiny tube into a vein in your arm (drip). It can only be given when your waters have broken.
The drip is increased very slowly until your uterus is contracting regularly and strongly. Women respond differently to how well the drip works on contractions and it also depends upon how ready your body is for the labour process.
During labour, your baby’s heart rate will be monitored continuously by a cardiotocography (CTG). Your ability to walk around will be limited by the drip and monitor, although you may choose to stand up or sit on a chair or birthing ball.
The Syntocinon® drip is the main form of induction when your waters have broken naturally and you do not go into labour.
We will endeavour to induce labour by 24 hours following rupture of membranes, however this may not always be possible. Please be assured that all decisions are made with regards to the safety of your baby and you. If your induction is delayed, you will be asked to come to the hospital Antenatal Clinic/Day Unit so that your baby and you can be assessed and monitored.
Can there be any complications or risks?
Cervical Ripening Balloon Catheter
The procedure can be uncomfortable but it should not be very painful. You may get strong period cramps after the balloon is inserted, usually these die off after a few hours. It is suggested that you have some pain relief ready at home for this. Paracetamol or Co-codamol is fine to take in pregnancy. We may give you some strong Co-codamol to take home with you if you need it.
There is a very small risk of infection. If an infection is suspected, your baby will need to be delivered by the quickest possible method. So, it is VERY important to let us know if you think your waters have broken while the balloon is still in.
Prostaglandin (Prostin®)
Inserting the prostaglandin pessary can be uncomfortable. Prostaglandin can cause dryness and soreness in and around the vagina. It can also cause strong contractions, which can be painful; having these contractions does not always mean you are in labour. Your midwife will discuss ways to help you manage this.
On rare occasions prostaglandins can cause the uterus to contract too frequently and this may affect the pattern of your baby’s heartbeat. This is usually treated by giving a drug that helps the uterus to relax. Sometimes the uterus continues to contract too frequently, which may mean an emergency caesarean section is necessary.
Oxytocin (Syntocinon®)
As with prostaglandin, the main risk is that the uterus can contract too strongly/frequently and affect the baby’s heartbeat. Reducing the rate of the Oxytocin can have an immediate effect on easing the contractions, which will improve the baby’s heartbeat. If the baby’s heartbeat does not recover, the senior doctors will decide what is required. This may mean an emergency caesarean section is necessary.
What happens if induction of labour fails?
In a small number of cases induction of labour is not successful following repeated attempts. Your management will then be discussed with your consultant obstetrician and a plan for birth put into place. It may be that a caesarean section is recommended.
How do I prepare for induction of labour?
Please read this information leaflet and share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are supporting you as the birth partner/s.
We recommend making family, especially children and those caring for them ,and friends aware that the procedure can take a long time (in some cases up to 10 days) before the baby is born.
It is also important that you are ready to come to the Labour Ward when called, otherwise you may lose your ‘slot’. Consider having someone on ‘standby’ to look after children or pets and someone to bring you into hospital.
You may want to nominate one person to give the rest of the family updates on how things are progressing.
You can bring one birth partner to Induction Clinic with you.
It is advisable to wear loose clothing when coming to the Induction Clinic as it will be more comfortable when you are being examined.
If you are admitted to the Antenatal Ward (Maple Ward), wear clothes you are comfortable in. It is not necessary to wear night clothes in the day as we actively encourage you to be mobile, depending on any medical condition you may have.
You may bring a book, magazines and games to keep you occupied due to the length of time the procedure may take.
There are television and telephone consoles by each bed and there is a secure mobile phone charging station on the ward. MOBILE PHONES SHOULD NOT BE CHARGED BY THE BED.
Please ask the ward staff for current visiting times.
Introduction
This leaflet has been produced to give you general information about the procedure of induction of labour. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your midwife or doctor but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with the midwife or doctor.
There is also a video on the Maternity service website that gives you a ‘virtual tour’ of the clinic and what we do: https://www.hey.nhs.uk/maternity/induction-of-labour-clinic/
What is induction of Labour?
In order for a baby to be born the cervix (the neck or opening to the womb) has to change from being closed, long and hard (touching the end of your nose, is similar to feeling the cervix) to being short, soft and starting to open. When that change happens, the strong ‘working’ contractions of labour start. Your womb has a powerful muscular wall that tightens and then relaxes; these contractions gradually open your cervix. In most pregnancies this starts naturally between 37 – 42 weeks and is called ‘spontaneous labour’.
Induction of labour is a process that tries to start labour artificially by opening and softening the cervix enough to break the waters around the baby. The final stage of the process is breaking the water around the baby and, if necessary, using a hormone ‘drip’ to start contractions.
When might I be offered induction of labour?
There are three main reasons why induction of labour (IOL) is offered:
- Prolonged pregnancy – pregnancy that continues after 41 weeks.
After 41 weeks there is a slight increase in the risk of your baby developing health problems. We therefore recommend Induction of labour between 41 and 42 weeks. - Pre-labour rupture of membranes – (the waters around the baby breaking) if spontaneous labour does not happen approximately 24 hours after the waters break there is a small risk of infection to the mother and /or the baby.
- Medical reasons – If it is felt that your health or your baby’s health is at increased risk if the pregnancy continues
Can I choose not to be induced?
You will be given information about the risks and benefits of IOL and the evidence behind why we would recommend IOL for your particular circumstances.
You will be given time to ask questions and to make your decision.
If you decide you do not want to be induced, you should tell your midwife or doctor and the reason why you do not want to be induced will be discussed. In partnership with you we will make a plan that supports your decision.
It is usually recommended that we keep a closer eye on you and your baby in these circumstances. How often you come to the hospital for checks depends on your situation. The midwife or doctor will discuss this with you.
Membrane Sweep (stretch and sweep)
Once you have reached your due date, you will be offered a membrane sweep at around 40 weeks, which may be followed by another at 41 weeks. This procedure has been shown to increase the chances of labour starting naturally within 48 hours of the procedure and can reduce the need for other methods of induction of labour.
You will also be offered a membrane sweep if induction of labour is being done for medical reasons. The timing will be advised by the doctor responsible for your care.
A stretch and sweep is a vaginal examination that can be carried out at home or at an Antenatal Clinic. The procedure involves the doctor or midwife putting two fingers inside your cervix and making a circular sweeping movement to separate the membranes from the cervix. This increases the production of hormones called prostaglandins which can encourage labour to start.
There may be some discomfort or bleeding but it will not cause any harm to you or your baby. It will not increase the chance of you or your baby getting an infection.
Sometimes the cervix is not ready to have a membrane sweep performed. This is not a problem, it simply means the body has not started to produce the hormones and chemicals needed to change the cervix at the time the membrane sweep was attempted.
Where will labour be induced?
The majority of women will be managed in an outpatient setting. All women come to an Induction of Labour Clinic to have the procedure started.
Most women will be able to go home afterwards, but sometimes you will have to stay in hospital because of medical reasons or the method of induction being used. You may want to pack a birth bag and either bring it with you or have it available in your car. Please DO NOT bring a car seat with you. It is unlikely that baby will be born on the day your induction is started.
If your cervix is already favourable to have the waters around your baby broken when you come to clinic, or if the waters have already broken you will be placed on the waiting list to be induced on the Labour Ward.
Please be aware that artificially breaking the water around the baby can only be done on Labour Ward.
Admission to the Labour Ward will be managed according to individual needs and this may happen straight away or more likely you will be asked to wait at home until you are called to attend Labour Ward.
It is very important that we have the correct contact details for you and you keep your phone switched on all the time as you can be called to Labour Ward at any time day or night.
While you are waiting at home you will be asked to come into the IOL Clinic to monitor you and your baby. How often depends upon why you are being induced.
An outpatient induction of labour:
- Reduces the amount of time you will need to stay in hospital before your labour begins.
- Allows you to stay at home which evidence has shown helps labour to progress as you are in a familiar place.
- Makes the process of induction as close as possible to going into labour naturally
Your midwife or doctor will assess if you are suitable for outpatient induction of labour and discuss this with you.
At very busy times, the start of the induction process may be delayed. Very rarely it may be delayed for over 48 hours. If you are at home, you may be advised to come in to the Induction Clinic to have an antenatal review and to monitor your baby with a cardiotocograph (CTG) machine. You will be able to go home afterwards if there are no concerns about you or your baby.
What will happen?
When you come to clinic the midwife will introduce themselves and discuss everything with you to make sure you understand the procedure. Please feel free to ask any questions or voice any concerns or anxieties. We understand that Induction of Labour can make you feel anxious and scared and it is sometimes difficult to remember any questions or things you want to say so it might be useful to write down anything you want to discuss. We are here to listen to you and help if we can..
When you arrive, the midwife will do a full antenatal check on you and your baby. Your baby’s heartbeat will be monitored using a cardiotograph (CTG) machine that gives a paper recording of the heartbeat.
You will have a vaginal examination to determine if your cervix is ready to be able to break your waters (Artificial Rupture of Membranes/ ARM). In order to break the waters your cervix needs to have changed from being long, closed and hard to being thin, soft and stretchy and starting to dilate (open up). This naturally happens at the end of the pregnancy when the body starts to produce the hormones that start labour but it might not have started to happen if labour is induced before your due date.
Methods used to prepare the cervix
These are used to soften and open the cervix in order to be able to ‘break the waters’ around the baby. They may sometimes cause contractions to start as well.
You may need just one or all of these methods.
Cervical Ripening Balloon Catheter
The balloon catheter is the only method used for outpatient induction of labour. This is because it has minimal side effects and does not need you to be monitored as closely as when using a medical method.
The procedure involves a catheter (a soft silicone tube) being inserted into your cervix. It has a balloon near the tip and when it is in place the balloon is filled with a sterile saline (salt water) fluid. The catheter stays in for up to 24 hours, with the balloon putting gentle pressure on your cervix. This should soften and open your cervix enough to be able to break the waters around your baby or it may start labour. It is important to realise that this does not happen for everyone and you may need to progress to other methods.
If we are unable to insert a balloon catheter then we will go straight to the next method.
Sometimes a double balloon is used especially if your cervix is very long or hard. It works the same as a single balloon.
The balloon catheter may fall out by itself or will be removed by a midwife the following day.
Going home after cervical ripening balloon catheter
During the time you are at home, you can do things as you would normally, for example, showering, bathing or walking. However, please avoid intercourse. After going to the toilet please wash your hands, make sure the catheter is clean and change underwear regularly.
You are likely to get strong period-type cramps after the balloon has been inserted. These will usually wear off after 6-8 hours. You will be advised to take pain relief and try things like a warm bath or a cold compress.
If you have any of the following:
- Bleeding enough to soak through a sanitary towel
- Contractions
- Concerns about the baby’s movements
Or
- You feel unwell
- The waters around the baby break.
- The balloon falls out
You are advised to call Maple Ward on (01482) 607779. A midwife will talk with you and advise you what you need to do.
Prostaglandin
Prostaglandin is a hormone that is naturally produced by the body. It is involved in starting labour. We use two methods to deliver an artificial version of prostaglandin.
- A pessary known as ‘Propess’® is inserted into the vagina and place behind the cervix. It has tape attached so it can be removed easily. It releases the hormone slowly over 24 hours but will be removed earlier if labour starts or there are any concerns about you or your baby’s health.
- A tablet called ‘Prostin’® is inserted into the vagina and next to the cervix. You will be re-examined six hours after the first tablet; if the cervix is still not ready for the waters to be broken or you have not started in labour then a second Prostin® tablet will be inserted into the vagina.
You will have to stay in hospital if these methods are used, as your baby will need to be monitored every eight hours. Between monitoring, you will be encouraged to walk about or use the ‘birthing balls’, as being active can help to encourage labour to start.
It is important to be aware that the process of softening and opening the cervix can take up to three days if you are over 41 weeks and up to five days if we are inducing you earlier than 41 weeks. It is also important to know that it may fail completely.
You may become favourable to have your waters broken (ARM) at any point during the process. When that happens the Induction process has worked and you will be placed on a waiting list to go to the labour ward to have your waters broken.
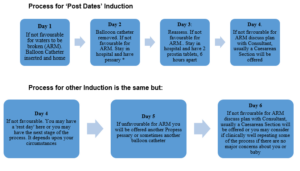
Process for IOL.
|
Previous Caesarean Section
If you have had a previous Caesarean Section we have to be very careful with prostaglandin as it increases the chance of the scar separating or tearing.
You will only be offered the Balloon Catheter. You may be offered another one if the first one is not successful.
What happens next
When the cervix is favourable to have the waters around the baby broken, known as an Artificial Rupture of Membranes (ARM), you may be able to go home and wait to be contacted by the Labour Ward with a time for admission.
THIS CAN TAKE UP TO FIVE DAYS. The consultant in charge of the Labour Ward will make a decision about when to admit you to the Labour Ward based on medical needs and at all times keeping in mind the safety of your baby and you. If you are being induced because you are Post-dates (41 weeks or over) you will be a priority to go to Labour ward.
If you are being induced as an outpatient, this will NOT affect the decision about when you will be admitted to the Labour Ward.
During this ‘waiting time’ you will be offered appointments in the Induction Clinic so we can monitor your baby and yourself and give membrane sweeps if you want. How often this happens will depend on the reason why you are being induced.
If your waters break by themselves then you may be able to wait to see if you go into labour. If you do not, then labour will be induced with the hormone drip approximately 24 hours following the waters’ breaking.
If you go into labour by yourself, you are no longer on a ‘waiting list’ but will be admitted to the Labour Ward or Midwifery -Led Unit when labour is established.
What happens if induction of labour fails?
In a small number of cases induction of labour is not successful following repeated attempts. If the process has failed you will be offered a planned Caesarean Section. Your Consultant and the ward staff will arrange all this for you.
What happens on the Labour Ward
Artificial rupture of the membranes (ARM)
When the cervix is soft, open to around two to three centimetres and the baby’s head has gone down into your pelvis, it should be possible to ‘break the waters’ around the baby.
This procedure is carried out by using a small plastic hook which releases the water and allows the pressure of the baby’s head to press on the cervix and stimulate contractions. It will not harm you or your baby. The procedure may be uncomfortable but it should not be painful.
You may be given some time to see if contractions start or we may use an artificial hormone called Syntocinon® straight away.
Oxytocin (Syntocinon®)
This is an artificial form of the hormone that causes your uterus (womb) to start having contractions.
It is given through a tiny tube into a vein in your arm (drip). It can only be given when your waters have broken.
The drip is increased very slowly until your uterus is contracting regularly and strongly. Women respond differently to how well the drip works on contractions and it also depends upon how ready your body is for the labour process.
During labour, your baby’s heart rate will be monitored continuously by a cardiotocography (CTG). Your ability to walk around will be limited by the drip and monitor, although you may choose to stand up or sit on a chair or birthing ball.
The Syntocinon® drip is the main form of induction when your waters have broken naturally and you do not go into labour.
We will endeavour to induce labour by 24 hours following rupture of membranes, however this may not always be possible. Please be assured that all decisions are made with regards to the safety of your baby and you. If your induction is delayed, you will be asked to come to the hospital Antenatal Clinic/Day Unit so that your baby and you can be assessed and monitored.
Can there be any complications or risks?
Cervical Ripening Balloon Catheter
The procedure can be uncomfortable but it should not be very painful. You may get very strong period cramps after the balloon is inserted, usually these die off about 6-8 hours after the balloon is inserted. It usually means that the balloon is working and ripening the cervix. It is suggested that you have some pain relief ready at home for this. Paracetamol or Co-codamol is fine to take in pregnancy. We may give you some strong Co-codamol to take home with you if you need it.
There is a very small risk of infection. If an infection is suspected, your baby will need to be delivered by the quickest possible method. So, it is VERY important to let us know if you think your waters have broken while the balloon is still in.
Prostaglandin (Prostin®)
Inserting the prostaglandin pessary can be uncomfortable. Prostaglandin can cause dryness and soreness in and around the vagina. It can also cause strong contractions, which can be painful; having these contractions does not always mean you are in labour. Your midwife will discuss ways to help you manage this.
On rare occasions prostaglandins can cause the uterus to contract too frequently and this may affect the pattern of your baby’s heartbeat. This is usually treated by giving a drug that helps the uterus to relax. Sometimes the uterus continues to contract too frequently, which may mean an emergency caesarean section is necessary.
Oxytocin (Syntocinon®)
As with prostaglandin, the main risk is that the uterus can contract too strongly/frequently and affect the baby’s heartbeat. Reducing the rate of the Oxytocin can have an immediate effect on easing the contractions, which will improve the baby’s heartbeat. If the baby’s heartbeat does not recover, the senior doctors will decide what is required. This may mean an emergency caesarean section is necessary.
How do I prepare for induction of labour?
Please read this information leaflet and share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are supporting you as the birth partner/s.
We recommend making family, especially children and those caring for them ,and friends aware that the procedure can take a long time (in some cases up to 10 days) before the baby is born.
It is also important that you are ready to come to the Labour Ward when called, otherwise you may lose your ‘slot’. Consider having someone on ‘standby’ to look after children or pets and someone to bring you into hospital.
You may want to nominate one person to give the rest of the family updates on how things are progressing.
You can bring one birth partner to Induction Clinic with you.
It is advisable to wear loose clothing when coming to the Induction Clinic as it will be more comfortable when you are being examined.
If you are admitted to the Antenatal Ward (Maple Ward), wear clothes you are comfortable in. It is not necessary to wear night clothes in the day as we actively encourage you to be mobile, depending on any medical condition you may have.
You may bring a book, magazines and games to keep you occupied due to the length of time the procedure may take.
There are television and telephone consoles by each bed and there is a secure mobile phone charging station on the ward. MOBILE PHONES SHOULD NOT BE CHARGED BY THE BED.
Please ask the ward staff for current visiting times.
| We understand that Induction of Labour can be a lengthy and sometimes stressful procedure. Please note that verbal abuse to hospital staff will not be tolerated. Instead, don’t hesitate to talk about your worries or concerns with the staff on the ward. We are here to help you and your family to have the best possible birth experience whatever the circumstances.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact Maple Ward (01482) 607438 |
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

