- Reference Number: HEY-491/2018
- Departments: Maternity Services
- Last Updated: 3 May 2022
Introduction
Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor or midwife, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
What is Mifepristone?
Mifepristone is a tablet which acts by blocking the effects of progesterone, a hormone which is needed for a pregnancy to continue. It makes the uterus (womb) sensitive to contractions and helps in the next process of inducing labour, by softening the cervix (neck of the womb).
It is important to inform you that Mifepristone does not have a UK licence for use in pregnancy but is a recognised and approved drug of choice for ending a pregnancy. It is proven to work effectively. This can be discussed fully with your doctor or midwife.
Can there be any complications or risks?
In some circumstances this treatment may be unsuitable for you so please tell the doctor if:
- You have a heart complaint
- You have risk factors for heart disease such as high blood pressure or cholesterol (increased fat levels in your blood)
- You suffer from asthma
- You suffer from an illness that may affect the clotting of your blood
- You have kidney or liver disease
Some medicines containing the following ingredients can interfere with the action of the mifepristone therefore please tell the doctor if you are taking or have recently taken any of the following:
- Corticosteroids (used in the treatment of asthma or other inflammatory treatments)
- Erythromycin, Rifampicin (antibiotics)
- St John’s Wort (natural remedy used in the treatment of mild depression)
- Phenytoin, phenobarbital, carbamazepine (used in the treatment of seizures: epilepsy)
- Ketoconazole, Itraconazole (used in antifungal treatment)
Do not take any anti-inflammatory pain killers after taking mifepristone such as:
- Ibuprofen (Nurofen)
- Aspirin
- Diclofenac
Diet – Grapefruit juice should not be taken when you are treated with mifepristone.
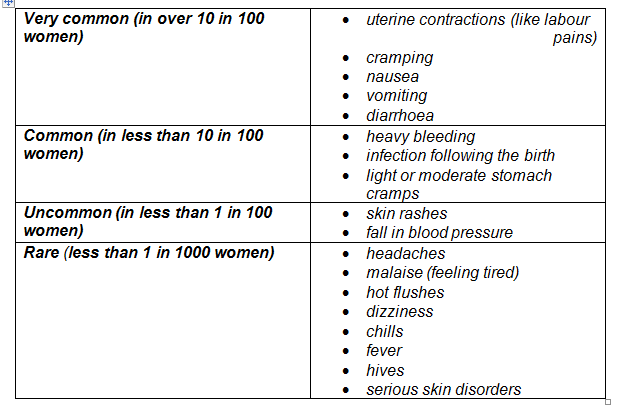
Possible Side Effects
Like all medicines, mifepristone can cause side effects, although not everybody gets them.
What will happen?
At the Antenatal Clinic
A midwife will check your personal details, document any allergies and discuss any concerns or queries you may have. It is important to say if you are unsure about anything at this point. The midwife will then take your blood pressure, temperature, pulse and respirations (vital signs).
Taking Mifepristone tablets
The mifepristone tablets can be swallowed with water. Sometimes mifepristone can make you feel sick and nauseous, so it is important to remain in the department for up to an hour after taking the tablets. The midwife will recheck your vital signs before you go home.
Admission to the Labour and Delivery Suite
The midwife will give you a date and estimated time to come into the Labour and Delivery Suite for the second part of the process which is usually around 48 hours after taking the Mifepristone. We ask that you ring the Labour and Delivery Suite in advance of your admission, to confirm a mutually suitable time for you to come in.
Pleased be assured that a designated midwife will be available at all times to support you during your time on the Labour and Delivery Suite. Additionally the bereavement midwife will be available to provide support during your time in hospital and following your discharge home.
What happens after taking the Mifepristone?
If you are sick within two hours of taking the tablets, please telephone the Antenatal Clinic, Antenatal Day Unit, or the Labour and Delivery Suite for advice. The telephone numbers are on the back of this leaflet.
You may experience some backache or mild period type pains prior to your admission to the Labour and Delivery Suite. This can be helped by taking paracetamol. If the discomfort worsens or if you have any bleeding from the vagina, telephone the Labour and Delivery Suite and ask to speak to the Labour Ward Coordinator who will have your details and will be able to give you advice.
Whilst at home eat and drink as normal, try and rest and pack the things that you will need for your stay in hospital. The induction process can take anything from hours to a few days before the birth. Your family can come and visit/support you during this time.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact:
Labour and Delivery Suite on (01482) 604490 or 604390.
Antenatal Clinic (01482) 382623
Antenatal Day Unit (01482) 382729
Community Midwifes (01482) 382658
Bereavement Midwife (01482) 608962
This leaflet was produced by Hull University Teaching Hospital NHS Trust
Ref: HEY 491/2018 review November 2024
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.