- Reference Number: HEY-490/2023
- Departments: Maternity Services
- Last Updated: 1 March 2023
Introduction
This leaflet has been produced to give you information about 3rd and 4th degree tears. It is not intended to replace the discussion between you and your doctor or midwife, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with the doctor or midwife who is caring for you.
What is a tear?
As your baby is being delivered a tear can occur. A tear involves the skin and muscle of the perineum which is the area between your vagina and back passage (anus). A tear can also occur inside your vagina and in the labia (lips of the vagina).
What are the types of tear during childbirth?
Most women experience tears to some extent during childbirth as the baby stretches the vagina and perineum.
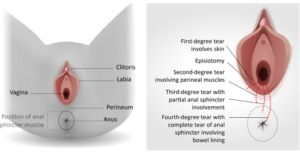
Most tears occur in the perineum, the area between the vaginal opening and the anus (back passage). They may be:
- 1st degree tears – Small, skin deep tear which usually heal naturally.
- 2nd degree tears – Deeper tears affecting the muscle of the perineum as well as the skin. These will require stitches.
When deeper tears occurred, they may be :
- 3rd degree tear – a tear that extends into the muscle that controls the anus (the anal sphincter)
- 4th degree tear – a tear extends further into the lining of the anus or rectum.
What is an episiotomy?
An episiotomy is a cut made by a healthcare professional through the vaginal wall and perineum. This may be done if your baby needs to be born more quickly or to make more space for your baby to be born. It is possible for an episiotomy to extend and become a deeper tear.
What is a rectal buttonhole?
This is a rare injury and occurs when the anal sphincter is not torn, but there is a hole between the back passage and the vagina. This means that wind and faeces may be passed through the vagina instead of via the anus. This is not normal, and if you experience this you should see your healthcare professional urgently.
In the UK, a 3rd or 4th degree tear (also known as obstetric anal sphincter injury – OASI) occurs in about 3 in100 women having a vaginal birth. It is more common with a first vaginal birth, occurring in 6 in100 women, compared with 2 in 100 women who have previously had a vaginal birth.
What happens after the birth?
Your obstetrician or midwife will examine your perineum and identify if any tears occurred. If they suspect a 3rd or 4th degree tear, or if you had an episiotomy (a cut), a detailed examination of your perineum and anus will be performed by the obstetrician, who will confirm the extent of the tear and provide information about surgery and treatment options available to you.
What happens next?
You will need an anaesthetic before any treatment can be given. This is usually an epidural or spinal anaesthesia. Rarely, you may need a general anaesthetic (where you are put to sleep). A midwife will be with you at all times during the surgery to support and answer any questions you may have.
Once you have your anaesthetic the obstetrician will start to suture (stitch) the tear. The surgery for 3rd or 4th tears usually takes place in the operating theatre.
What treatment will I be offered after surgery?
Below are the treatments you will be given following your surgery:
- Antibiotics – You will be given a single dose of antibiotic during surgery to reduce the risk of infection because the stitches are very close to the anus. You will also need to take a course of antibiotics following the surgery.
- Pain-relieving drugs – You will be offered one or more pain-relieving drugs such as paracetamol, ibuprofen or diclofenac to relieve any pain.
- Laxatives – You will be advised to take lactulose to make it easier and more comfortable to open your bowels.
- A drip – Fluids will be given in your arm until you feel able to eat and drink.
- You may have a urinary catheter – A (tube) in your bladder, for 12 – 24 hours to help you pass urine. This is usually kept in until you are able to walk to the toilet.
Will I be able to breastfeed ?
Yes. None of the treatments offered will prevent you from breastfeeding.
Prior to discharge from hospital
It is preferred but not essential that you have opened your bowels before you leave hospital.
What do I need to know about my stitches?
You will have stitches between your vagina and anus and also beneath your skin. They will eventually all dissolve (soften and fall out) and you may notice small threads in your pad or in the bath. You may be able to feel some of the stitches, especially those around the anus muscle, for up to 3 months.
After having any tear, you are likely to experience pain or soreness for 4–6 weeks after giving birth, particularly when walking or sitting. The stitches can irritate as healing takes place, but this is normal. Passing urine can cause stinging – pouring water over the area when urinating can help.
If you are worried about the way your wound is healing or if you notice any bleeding from the tear, any unpleasant smell or any increase in pain, you should see your healthcare professional. This might be a sign of infection and you may need some antibiotics to help it heal.
What do I need to know about my bowels?
Opening your bowels should not affect your stitches. For the first few days after your 3rd or 4th degree tear is repaired, control of your bowels may not be as good as before you had your baby. It is important to eat well and drink plenty of water to help avoid constipation. You should drink at least
2 litres of water every day and eat a healthy balanced diet (for instance fruit, vegetables, cereals and wholemeal bread).
When opening your bowels, the best position to sit in is with your feet on a stool to raise your knees above your hips (see image). This helps straighten out your bowels. Try to relax and rest your elbows on your knees. Bulge out your tummy by taking big abdominal breaths – this will help to expel your faeces without straining. Take your time and do not rush.
Caring for your wound or painful perineum
Your midwife will review your perineum when you get home and we would strongly advise you to consent to this review as they will look for signs of infection and to check if the wound is healing well.
Below are some important points to remember:
- Keep your wound clean.
- Wear breathable materials, like cotton and disposable briefs, and avoid tight clothing.
- Begin doing your pelvic floor exercises as soon as you can after birth this strengthens the muscles around the vagina and anus and help healing.
- Ensure you are comfortable when sitting to feed your baby, you may find it more comfortable feeding on your side.
To help with discomfort:
- You can use cold/ice packs. Do not apply directly onto the skin always wrap in a cloth/flannel and apply for 30 minutes every so often throughout the first few days.
- Take regular pain relief for the first two to three days if required. Paracetamol and ibuprofen are both safe while breast feeding but make sure you read and understand the label.
- You may find it helpful to pour luke warm water over your perineum during and after passing urine, to help reduce the stinging or use a shower head or bidet.
It is important to keep this area clean:
- Wash your hands before and after using the toilet.
- Wash your perineum after every visit to the toilet.
- Just pat/wipe the area dry with toilet paper. Always wipe, front to back to avoid contamination from your back passage.
- Change your sanitary towel regularly, at least every four hours. Ensure it is secured in place so it does not move around and cause further irritation.
- Use plain water to clean this area, you can have a bath or shower as usual and you may find this soothing. You do not need to add anything special to your bath to help with healing.
When can I have sex?
Many women are worried by the thought of having sexual intercourse again after they have given birth, particularly when they have experienced a3rd or 4th degree tear. Once your stitches have healed and bleeding has stopped, you can have sex again when it feels right for you and your partner.
Things to think about:
- Do not forget you can become pregnant the first time you have sex after the birth of your baby. Therefore it is important that you choose and use a suitable method of contraception. You can discuss your contraception options with your healthcare professional.
- Perineal massage, either on your own or with your partner, may help you feel more comfortable before you begin having sex again
- You may find it helpful to use a water soluble lubricating jelly if your vagina feels drier than usual, particularly if you are breastfeeding.
- Sex may be uncomfortable and feel different at first but the discomfort should not persist.
- You and your partner may be anxious and talking about these feelings may help, as it is important that you both feel ready and relaxed. If you continue to experience pain or discomfort, you should raise these concerns with your healthcare professional
What are the immediate and long term effects of 3rd and 4th degree tears?
Most women make a good recovery, particularly if the tear is recognised and repaired as early as possible.
6–8 in 10 women with a 3rd or 4th degree tear will have no long-lasting complications after it has been repaired and given time to heal. However during recovery some women may experience:
- Pain or soreness in the perineum.
- A feeling that they need to rush to the toilet to open their bowels urgently.
- Fear about future pregnancy and birth.
Very rarely, you may have a fistula (hole) between your anus and vagina after the tear has healed. This can be repaired by further surgery and will be fully explained to you.
Contact your midwife or general practitioner if:
- You start to feel unwell or have a temperature
- Your stitches become more painful, or smell offensive – these may be signs of an infection
- The area starts to throb or starts to swell
- Your stiches are coming apart and the tear is not healing.
- You have problems controlling your urine or bowels or flatus (passing wind).
- You need to rush to the toilet to open your bowels due to incontinence problems.
- You have any other worries or concerns.
What is anal incontinence?
Anal incontinence is when you have problems controlling your bowels. Symptoms include sudden, uncontrollable urges to open your bowels and not being able to control passing wind. You may also soil yourself or leak faeces. Most 3rd or 4th degree tears heal completely, but some women may experience these symptoms. It is important to talk about any concerns you have. Women with anal incontinence will be referred to a specialist team for treatment, which may include physiotherapy or surgery.
What should I expect when getting back to normal daily activities?
Every woman’s recovery will be slightly different, and what they view as normal daily activities will also differ. If you have had a 3rd or 4th degree tear, you should avoid strenuous activity or heavy lifting for 4–6 weeks. After 4–6 weeks, you can gradually increase your general activity.
Looking after a newborn baby and recovering from an operation for a perineal tear can be hard. Support from family and friends can really help you while your body gradually adjusts and gets better. If you continue to experience symptoms after 6 months, see your healthcare professional.
Experiencing complications when giving birth can be very distressing and disturbing, and for some women there is a risk of post-traumatic stress disorder (PTSD). Following a perineal tear, if you are developing anxiety, have low mood or feel that you need additional support, you should talk to your healthcare professional.
Your follow up appointment
You may be offered a follow up clinic appointment at the hospital 6 – 12 weeks after you gave birth to check that your wound is healing properly. You will be asked if you have any problems controlling your bowels: such as leakage of stool (faeces) or wind, urgency (rushing to the toilet) or pain when opening your bowels. You may be referred to a specialist if you do.
This follow up appointment also offers you the opportunity to discuss any concerns that you may have.
What about future birth plans?
If you have recovered well and do not have any symptoms, you may wish to consider a vaginal birth. If you continue to experience symptoms from the 3rd or 4th degree tear, you may be offered to consider a planned caesarean birth.
Currently, there is limited evidence as to whether or not you are at increased risk of having another 3rd or 4th degree tear. It is suggested that women who have had a 3rd or 4th degree tear in their first birth have a 7 to 10 in100 chance of having a similar tear in their next vaginal birth. Risk factors for having a repeat 3rd or 4th degree tear include having a forceps birth, your baby being born heavier than 4kg and being of Asian ethnicity.
You will be able to discuss your options for future births at your follow-up appointment or early in your next pregnancy. Your healthcare professional will explore your individual experience and preferences so that you can make the decision that is right for you.
Contact numbers and further information
Further information about 3rd and 4th degree tears can be found at www.rcog.org.uk.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Community Midwives on telephone number: (01482) 382758.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

