- Reference Number: HEY-092/2023
- Departments: GI Physiology
- Last Updated: 24 July 2023
Introduction
This leaflet has been produced to give you general information about your upcoming hydrogen breath test. Most of your questions should be answered by this leaflet. If after reading it you have any concerns or would like further explanation, please contact the Department of GI Physiology directly on 01482 624036.
What is a Hydrogen Breath Test?
A hydrogen breath test is a non-invasive and safe test used to investigate intestinal disorders. To perform the test, you will be asked to provide a breath sample by blowing into a hand-held hydrogen breath test machine. You will then be given a sugar solution to drink, and further breath samples will be taken at regular intervals for up to 4 hours while the test solution travels through your digestive system.
Why do I need a Hydrogen Breath Test?
A hydrogen breath test can be used to detect abnormal bacterial growth in your small intestine. It is normal for bacteria to be found in your large intestine, where they aid digestion. However, sometimes bacteria can grow in the small intestine and interfere with the digestion of food. This is known as small intestinal bacterial overgrowth (SIBO). You will first attend the department for a simple breath sample, to determine which type of test you will need.
The SIBO test will then be carried out on another day using a solution containing glucose.
A hydrogen breath test can also provide information about the digestion of certain sugars, to help determine if you are intolerant to them (or cannot digest them). For example, people who have a lactose intolerance may develop symptoms after consuming dairy products, and people who have a fructose intolerance may develop symptoms after consuming fruit. If you have been referred for a lactose or fructose hydrogen breath test, you will need a test to rule out small intestinal bacterial overgrowth first (as SIBO can lead to a false lactose or fructose test result).
Can there be any complications or risks?
Hydrogen breath tests are considered very safe. In rare cases, the test sugar solution can cause loose stools. You may also find that drinking the test sugar solution triggers your usual symptoms.
How do I prepare for the Hydrogen Breath Test?
Please read this information leaflet carefully. If you wish, feel free to share the information with friends or family so that they can be of help and support.
4 weeks before your test:
- You should not take any antibiotics. If you have to take antibiotics during the 4 weeks before your appointment, please call the department to re-book the test.
1 week before your test:
- You should not undergo any test that requires cleansing of the bowel such as a colonoscopy, barium enema or colonic irrigation.
- Do not take any laxatives, stool softeners, stool bulking agents or any medication used to treat constipation.
- Do not take any probiotic yoghurts / probiotic supplements.
1 day before your test:
- The day before your test, please only eat the food items on the menu below.
If you are diabetic, please telephone the department for advice on 01482 624036.
Please note: Dairy products of any kind (including butter/spreads) are not allowed. The order of the meals may be changed, but it is essential that you do not eat or drink anything other than the foods and drinks listed below.
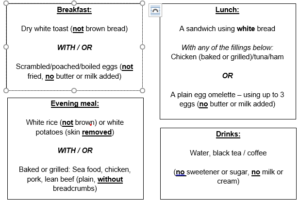
Do not eat anything from 6pm onwards the day before the test. Water is allowed the night before the test (and only a little water on the morning of the test).
On the day of your test:
- You should not eat anything in the morning (only a little water is allowed).
- Do not eat, drink, chew gum, eat breath mints/sweets or smoke cigarettes (including e-cigarettes) before or during the test.
- Do not sleep or exercise while the test is being carried out, as this can interfere with the result.
What will happen?
You should go to the Department of GI Physiology, next to Ward 14 at Castle Hill Hospital.
You do not need to be accompanied by a family member or friend for this appointment. However, there is plenty of seating in the waiting area should you wish to bring someone with you for support.
A member of staff from the department will explain the hydrogen breath test to you on the day of your test. This is to ensure that you understand the test and any implications. You will be asked to sign a consent form if you agree to have the test carried out. A member of staff from the department will then start the test.
The test is very easily performed. You will be asked to provide a breath sample by blowing out into a hand-held hydrogen breath test machine. The breath sample is collected with you blowing out at your normal rate, so this will not make you short of breath. Provided you have fasted correctly and have not smoked, the first reading should be very low. If the first reading is excessively high, we may have to ask you to return in a few hours, or re-book the test for another day.
You will then be given the test solution to drink, and further breath samples will be taken at regular intervals for up to 4 hours while the test solution travels through your digestive system. You may wish to bring some reading material with you for the duration of the test, and free Wi-Fi is available in the department.
After the test has finished, you may go home / to work and resume your normal diet. If further appointments are required for additional hydrogen breath tests, this will be arranged with you on the day.
What will happen afterwards?
A report of the results will be sent to the consultant in charge of your care, who will plan an appropriate treatment.
Should you require further information or advice, please do contact the GI Physiology Department on 01482 624036
This leaflet was produced by the Department of GI Physiology, Hull University Teaching Hospitals NHS Trust and will be reviewed in July 2026.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

