- Reference Number: HEY-841/2022
- Departments: Major Trauma
- Last Updated: 1 May 2022


Introduction to Hull Royal Infirmary
Welcome to Hull Royal Infirmary Major Trauma Centre
We hope that this booklet provides you with information necessary for you, or your relatives during your stay at Hull Royal Infirmary. If you require further information on topics that are not covered in this booklet, please do not hesitate in speaking to a member of staff in the department of your inpatient stay.
Relatives, please be advised that if you are making a telephone enquiry to the hospital to discuss an inpatient, only limited information can be passed over the telephone due to the Data Protection Act (2013).
The Data Protection Act (2013) ensures that patient confidentiality is paramount and therefore protection of confidential information is maintained.
Key Workers
Whilst an inpatient at Hull Royal Infirmary, you will be designated a key worker. The key worker role is designed to be the one point of contact for both the patient and relatives during the hospital stay and should be able to inform you all of relevant information involving your care and plans for discharge.
Your key worker will be one of the Major Trauma Coordinators and can be directly contacted on 07717 541 803.
What is a Major Trauma?
Major trauma is a term used to describe any physical injury which can have potential serious complications. A typical example of this term would be an individual involved in a road traffic collision (RTC) with complex injuries and needs; a fall from a significant height or an assault causing serious injuries.
Due to the variable nature of this term, major trauma can be further categorised to describe what type of injury you or your relative has suffered such as:
- Blunt force trauma – a non-penetrating external or internal injury caused by blunt force
- Penetrating trauma – an injury that penetrates through the skin to a space or organ within the body
- Orthopaedic trauma – injuries involving the musculoskeletal system
What is a Major Trauma Centre?
Although all hospitals can provide a range of treatments and cares, it is of utmost importance to provide major trauma patients with specialised care 24 hours a day. These hospitals are known as Major Trauma Centres (MTCs) and can provide the necessary multi-speciality care required for individuals.
Within an MTC, medical interventions can be found from specialities such as Emergency Medicine, Intensive Care, Orthopaedics, Neurosurgery, General Surgery, Vascular Surgery, Plastic Surgery, Interventional Radiology and Rehabilitation Medicine.
Across England there are 8 Adult Major Trauma Centres, of which Hull Royal Infirmary is one. There are a further 12 Adult and Paediatric Centres, 4 Paediatric Centres and 2 Collaborative Centres.
Each Major Trauma Centre is affiliated with its own Trauma Units. When combined, these form a Major Trauma Network. Our network is known as the North Yorkshire and Humberside Operational Delivery Network and comprises of:
- Hull Royal Infirmary
- Diana Princess of Wales Hospital (DPOW) — Grimsby
- Scarborough Hospital
- Scunthorpe General Hospital
- York Teaching Hospital
Our Major Trauma Centre, Trauma Units and Network
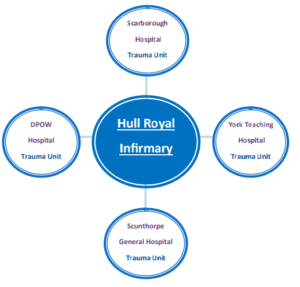
Above: Network of Trauma Units and the Major Trauma Centre for North Yorkshire & Humberside. Please note that Minor Injuries Units are not part of the Major Trauma Network, but will transfer any patient to the appropriate hospital should a patient self-present
Why have I been admitted to Hull Royal Infirmary?
Each Major Trauma Centre and Trauma Unit work very closely with their pre-hospital care teams. Within our Network, we engage with the following services:
- British Association for Immediate Care (BASICS)
- East Midlands Ambulance Service
- HM Coastguard Search and Rescue
- Lincolnshire First Responders (LIVES)
- Lincolnshire and Nottingham Air Ambulance
- The Air Ambulance Service
- Yorkshire Ambulance Service and Yorkshire Air Ambulance
On attending an incident, the pre-hospital teams conduct a multifactorial assessment which evaluates the current and potential risks to the patient. The assessment includes taking clinical observations and identifying immediate issues, such as obvious injuries that need instant attention. If the crew are concerned with any of these measures, or the patient fulfils specific criteria, they will Pre-Alert the Emergency Department at Hull Royal Infirmary.
You may find that you or your relative were taken to a Trauma Unit before arriving at Hull Royal Infirmary. Depending on the severity of the injuries sustained or condition of the patient, it may be that stabilisation is required before continuing the journey. It may also be that should the journey take longer that 60 minutes, it is required that an assessment take place before reaching us. Alternatively, you may have been admitted to a Trauma Unit only to find that the injuries you have sustained now require specialist treatment that can only be carried out at ull Royal Infirmary.
What happens on my arrival at Hull Royal Infirmary?
As previously mentioned, the Pre-Hospital Team will alert the Emergency Department staff that a patient is on their way who fulfils criteria set on the Major Trauma Triage Tool.
Once this alert is received in the Emergency Department, a trauma call is likely to be activated. You will be met by one of three teams; an Emergency Department Trauma Team that consists just of those based in that department, or a Hospital Trauma or Code Red Team that will have the following people in attendance:
- Anaesthetist and Airways Assistant
- Emergency Department Consultant
- Emergency Department Senior Doctor
- Emergency Department Nurse(s)
- General Surgeon
- Major Trauma Coordinator and Consultant
- Orthopaedic Surgeon
- Radiologist and Radiographer
There are occasions where more than one doctor from each speciality attend the call; this is perfectly normal and is controlled by the team leader.
The aim of the Hospital Trauma Team activation is that all main specialities are present for the arrival so that we can provide the patient with the best care and treatment as quickly as possible.
The immediate investigations and treatment the patient receives will depend on the injuries and their severity. Each patient will receive what we call a Primary and Secondary Survey. These are explained further on in this booklet.
Clinical assessments on arrival
If you or your relative activated a trauma call, it is normal to have the following assessments upon your arrival:
The Primary Survey is a quick and efficient assessment completed by senior medical staff, aiming to identify any injuries that are life-threatening or of concern. Anything identified at this stage is immediately treated. Examples of this may be that a chest drain is inserted to allow adequate breathing, a blood transfusion may be swiftly administered in order to maintain an adequate blood pressure, or a breathing tube may be placed if there is a low conscious level.
Within this period other members of the team are jointly working alongside each other to gain Intravenous access (a cannula into the vein) to administer necessary fluid, blood or medication. Blood samples will be sent and arrangements for further investigations such as CT scans are commenced here.
The Secondary Survey takes place once all immediate risks are being managed. This assessment checks all of your systems from head-to-toe in order to identify anything that could have been missed, or that was not deemed life-threatening during the initial assessment. An example is to X-ray a fractured limb and place this within a cast, or checking if there is sensory loss to limbs should there be a neck or back injury. If required, further specialist teams are called at this point for their assessment. If an admission is necessary, a speciality team is allocated to you in the Emergency Department.
If you are admitted, the Major Trauma Team will visit you on the ward to perform a Tertiary Survey. In essence, this is a repeat of the secondary survey to ensure that no further injuries or concerns have developed some 24 plus hours later.
te support for going home.
If you feel that you or your relative needs any support, or foresee potential issues on discharge, please inform the staff as soon as possible.
Your Major Trauma Team
In addition to the specialist team you have been admitted under, and the ward nursing and therapist team, you should be seen every weekday by the Major Trauma Consultant. A number of Consultants undertake this role from a variety of specialities to ensure your care is well managed and when senior input is required across a variety of specialities they are able to facilitate this.
We have a team of specialist nurses, Major Trauma Coordinators, who you will meet during your admission. They are often part of the ‘Trauma Team’ who managed your care in the Emergency Department. They work alongside the Major Trauma Consultant to ensure the various specialities involved in your care connect smoothly, plans are clear and you are kept informed about any developments in your care. This team of nurses follow you throughout your stay at Hull Royal Infirmary, whichever in-patient department you are in.
Enduring a Major Trauma can have a significant impact on your mental health. Because of this, within our team, we have a Major Trauma Clinical Psychologist. Once referred to the Psychology service our Psychologist will aim to see you during your inpatient stay and/or will provide information regarding where to seek help should you require it after your discharge.
A Chaplaincy Service is available 24 hours a day. If you feel that as a patient or a relative you would like to see a chaplain, please inform the staff who can contact the team on your behalf. Alternatively, you can ring the team within office hours on (01482) 675966, or via switchboard (01482) 875875 out of hours.
A chapel is situated on the ground floor at Hull Royal Infirmary and near to Ward 11 at Castle Hill Hospital should you wish to visit.
Whatever your religion, we can help find you a faith-specific representative to talk to.
The Multi-Disciplinary Team Involvement
Alongside the Medical and Nursing teams, an array of professionals work together in order to offer a thorough and appropriate care management pathway. The following list highlights just some of the professionals who work together in providing a Multi-Disciplinary Team:
- Acute Pain Services
- Clinical Pharmacists
- Clinical Psychology and Mental Health
- Dieticians and Speech and Language Therapists
- Major Trauma Consultants and Coordinators
- Occupational Therapists
- Physiotherapists
- Rehabilitation Consultants and Coordinators
- Social Workers, Specialist Nursing and Therapy groups
Throughout the hospital stay, patients may be referred to one, or many of our specialist professionals within the Multi-Disciplinary Team. As a service we do not only look at the current medical circumstances of an individual, but that of potential discharge problems and aim to provide both the patients and their relatives with the most appropriate support for going home.
If you feel that you or your relative needs any support, or foresee potential issues on discharge, please inform the staff as soon as possible.
What happens next?
This part really depends on what injuries the patient has sustained and to what extent, although ultimately all options have the same goal……
From admission to discharge, we aim to deliver the best care and treatment in the most timely and effective manner.
It is quite rare that an individual who triggers a Hospital Trauma Call is discharged home from the Emergency Department, but this does happen from time to time. If the injuries require further treatment or you or your relative’s condition is for further observation, then there are three main areas from the Emergency Department; Theatre, the Intensive Care Unit or the Major Trauma Ward. The Emergency Department staff will be able to give the you or your relatives an idea of where the admission is likely to be, or where the patient will go to after theatre.
It is sometimes necessary that once a patient has been assessed by the Trauma Team, they are required to transfer to Castle Hill Hospital for specialist Cardiothoracic treatment and surgery. Castle Hill Hospital is our second acute centre within the Hull University Teaching Hospitals NHS Trust, some six miles East.
Throughout the in-patient stay, overall medical care is provided by the Consultant-Led Speciality teams, but all patients are monitored by our Major Trauma Consultants and Major Trauma Coordinators. The consultant and coordinators will liaise with the appropriate wards and specialities to help support the recovery of you or your relative.
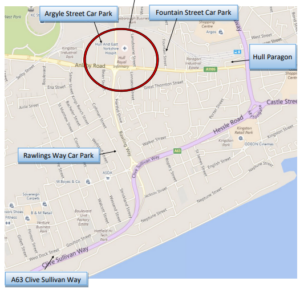
Car Parking
Car parking is available at our Argyle Street Car Park, using a barrier and pay as you leave arrangement. Current prices are listed below but please note these may be subject to change:
- Free for the first 30 minutes
- £2.00 for up to 1 hour
- £3.00 for 1 to 2 hours
- £5.00 for over 2 hours (maximum stay 24 hours)
- £10.00 Weekly parking pass (see below)
- £15.00 Fortnightly parking pass (see below)
- £20.00 Monthly parking pass (see below)
We understand that this car park is incredibly busy and do have private company car parks situated a few minutes walk from Hull Royal Infirmary. As shown on the map, Fountain Street and Rawlings Way car parks are conveniently situated nearby and reflect very similar prices to that of Argyle Street.
Another option if you are travelling from west of the A63 is the Priory Park, Park and Ride facility in Hessle. Situated a short drive from the hospital, you can park and travel to Hull Royal Infirmary for a small charge. Please note that buses run every 10 minutes between the hours of 07:00 – 19:00 Monday to Saturday. Enter postcode HU4 7DY into your navigation device.
We understand that it may become expensive when visiting your relative in hospital. In an attempt to alleviate financial pressure, the General Office can provide relatives with both a weekly and a monthly car parking pass for the use in Argyle Street Car Park. The General Office is located on the 3rd floor and can be contacted directly on (01482) 674218.
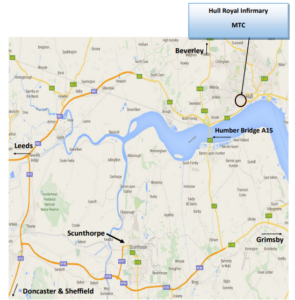
Hull Royal Infirmary MTC
Travelling to Hull Royal Infirmary
Contact Numbers and Visiting Times
Below are a few useful numbers that will take you directly where you need to be:
- Hull University Teaching Hospitals Switchboard (01482) 875875
- Major Trauma Ward (based on Ward 40) (01482) 675041 or 675040
- Intensive Care 1 at Hull Royal Infirmary (01482) 311727 or 311728
- Intensive Care 2 at Hull Royal Infirmary (01482) 311729 or 311733
- Intensive Care 1 at Castle Hill Hospital (01482) 461511
- Intensive Care 2 at Castle Hill Hospital (01482) 623179
- Patient Advice Liaison Service (PALS) (01482) 623065
Visiting Times of wards:
Please be advised that due to Covid-19, the hospital visiting policy changes on a regular basis. We advise that you call the ward prior to visiting to confirm the current policy and availability as these are subject to change.
Note: Due to some relatives travelling afar, it may be possible to extend your visiting hours. Please ring and ask the Nurse in Charge before you set off.
Food and Amenities
Food and drink is available from multiple places within the hospital site; please see below for opening times:
Nourish Restaurant (First Floor, Main Entrance, Hull Royal Infirmary) –
Monday to Friday – 07:00—19:30
Saturday and Sunday – 7.30 – 2.30
Costa Coffee (Ground Floor, Main Entrance, Hull Royal Infirmary) –
Monday to Friday – 7.30 – 7.30
Saturday, Sunday and Bank Holidays – 7.30 – 5.30
Fountains Café (Eye Hospital) –
Monday to Friday – 10:00 – 14:30
The Orchard Café (Women and Children’s Building) –
Monday to Friday – 08:00 – 17:00
Saturday and Sunday – 10:00—16:00
Pharmacy and Retail
Lloyds Outpatients Dispensary is situated in the main foyer within the Tower Block:
Lloyds outpatient services at Hull Royal Infirmary dispenses hospital outpatient prescriptions as well as IDL’s for children wards. It has a retail shop selling toiletries and a limited range of Pharmacy medicines (not for inpatient sale).
General Opening Hours
| Day | Opening | Closing |
|---|---|---|
| Monday – Friday | 8.30 am | 6.00 pm |
| Saturday | 10.00 am | 2.00 pm |
| Sunday | Closed | Closed |
| Christmas Day | Closed | Closed |
| All other bank holidays | 10.00 am | 2.00 pm |
WH Smith (main foyer within the Tower Block)
- 8.00am to 8.00pm Monday to Friday
- 9.00am to 7.00pm Saturday, Sunday and Bank Holidays
Services you may be able to access
Citizens Advice Bureau
We are able to ask a member of staff from the Citizens Advice Bureau to come and see you in hospital to assist with concerns you may have regarding benefits you may claim and any entitlements you may have if you are unable to work due to your injury. Please let us know if you would like to be referred.
Stewarts Law
Stewarts legal team work with the Trust and provide a free service to patients who have been on the Intensive Care Unit or who have had a Major Trauma. They can help with a variety of issues including:
- Welfare benefits
- Housing
- Financial issues (including if you are worried about debts accruing during your stay).
- Insurance and employment issues
- Powers of attorney
- Post discharge care
If you would like to be referred to this service please let the ward staff know.
Additional support services
There are a wide variety of organisations, charities and support networks potentially available to you. We have a noticeboard on ward 40 with more details or please ask a member of staff.
Rehabilitation and preparing for discharge
Rehabilitation is a key aspect to recovery for patients who have suffered Major Trauma and involvement from different professionals within the Major Trauma team will support patients during their hospital stay. The team meets on a daily basis Monday to Friday to discuss patients’ rehabilitation needs and plans necessary to help recovery. Physiotherapists and Occupational therapists are available to provide 7 day a week cover.
Where possible patients will be discharged straight home however this may not always be possible as some patients may need more time to recover from their injuries. If this is the case the team will talk to the patient about further rehabilitation and where this is likely to be based on where they live and what their needs are.
Rehabilitation will be planned with patients by staff involved in their care and will look at medical, physical, sensory and psychological needs. The team will complete their assessments and base treatment plans on the specific needs of each patient whilst in hospital as well as what they may require to support with planning for ongoing rehabilitation or discharge home (such as further inpatient or community rehabilitation, provision of equipment, a package of care to support at home)
If a patient’s local hospital is not Hull Royal Infirmary and further rehabilitation is required, support or equipment at home is needed or they have ongoing medical needs they may be transferred back to a more local hospital for this to be arranged. This is called repatriation. The teams in the local hospital will continue to help recovery and make plans for ongoing rehabilitation or discharge.
On discharge, if you have ongoing Rehabilitation needs you will receive a document with these details (known as a Rehab Prescription).
Accommodation
It may be necessary for relatives to stay close to the hospital and we recognise that some may have travelled a long distance to Hull Royal Infirmary. Therefore, below is a list of some local hotels and Bed and Breakfasts either within walking distance or a short car drive from the hospital:
Double Tree by Hilton Hotel— (01482) 755500
Holiday Inn Hull Marina – (01482) 692600
Holiday inn Express – (01482) 485700
Ibis Hotel – (01482) 947950
Kingston Theatre Hotel – (01482) 225828
Premier Inn Hull City Centre – 0333 003 1731
Royal Hull Hotel – 0871 222 1094
Travelodge Hull Central – 0871 984 6473
Should you need to stay nearby to Castle Hill Hospital, the following hotels are a short drive away:
Inn Keeper’s Lodge – (01482) 651518
Mecure Grange Park Hotel – (01482) 272673
Willerby Manor Hotel – (01482) 652616
Please Note: Limited accommodation is available at Hull Royal Infirmary in exceptional circumstances.
Patient Advice and Liaison Service (PALS) and Complaints
We hope that both the patients and relatives encounter no problems during their hospital stay. Not only do we aim to deliver the best care available, we also aim to maintain as good a relationship as possible with both patient and relatives alike.
If you feel that an issue has occurred, or that you are concerned with a matter then please raise this with the ward staff who will be able to help you. Should your query or issue remain unresolved, the Major Trauma Coordinator, as your key worker, should also be able to help and can be contacted on 07717 541 803.
If you remain dissatisfied with the service you have received, you have the right to contact our Patient Advice Liaison Service on:
(01482) 623065 or e-mail to hyp-tr.pals.mailbox@nhs.net
The Patient Advice and Liaison Service and Complaints Team work together in order to resolve concerns, provide answers to queries and to pass on complaints to the relevant teams within the Trust.
This booklet is for the use of Hull University Teaching Hospitals – Major Trauma Centre only.
Hull Royal Infirmary Major Trauma Centre Booklet
Created by Leah Dobson – Major Trauma Coordinator
Arranged & Edited by Alex Bampton – Admin Apprentice and the Major Trauma Team

May 2022
Pathway: MT/MTM/MTPatInfLeaf
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

