- Reference Number: HEY-291/2023
- Departments: GI Physiology
- Last Updated: 17 July 2023
Introduction
This leaflet has been produced to give you general information about your upcoming high resolution oesophageal manometry and 24-hour pH monitoring tests. Most of your questions should be answered by this leaflet. If after reading it you have any concerns or would like further explanation, please contact the Department of GI Physiology directly on 01482 624036.
What is High Resolution Oesophageal Manometry and 24 hour pH monitoring?
High resolution oesophageal manometry is a test that measures pressure in the oesophagus (food pipe) and sphincters (ring like muscles at either end of the oesophagus). The test is performed using a small probe (tube) with pressure sensors at 1 cm intervals, allowing pressure measurement along the whole oesophagus and both sphincters at the same time (please see the diagram below). This allows assessment of how well the muscles in the oesophagus and sphincters are working, and whether contractions within the oesophagus are co-ordinated.
24-hour pH monitoring measures the amount of acid coming up (refluxing) into the oesophagus from the stomach over a 24-hour period. This allows us to establish whether your symptoms are due to acid reflux.
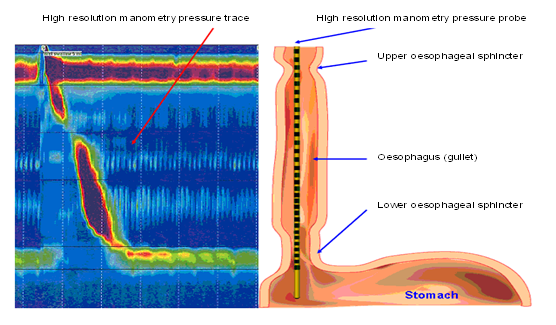
Diagram produced by the Hull & East Yorkshire Hospitals NHS Trust.
Why do I need High Resolution Oesophageal Manometry and 24 hour pH study?
Following discussion with your doctor, they advised that high resolution oesophageal manometry and 24-hour pH monitoring should be performed.
The tests provide valuable information regarding your condition and will help to decide what the best treatment is for you (for example, practical advice, medication or surgery). Unfortunately, there are no other tests available that will provide this information.
Our oesophageal manometry probe is the smallest and most sophisticated equipment available. This ensures that we can perform the test to the highest standards and make the whole procedure as quick and as comfortable as possible for you.
Can there be any complications or risks?
The risk of causing serious harm to you with this test is very rare. A minor side effect of oesophageal manometry and/or 24-hour pH monitoring can include a temporary runny nose (this can be caused by the tube inflaming the tissue inside your nose). It is likely that you will feel minor discomfort in your throat when the oesophageal manometry tube is in place, and very minor discomfort when the 24-hour tube is in place. Both of these effects usually disappear straight away when the tube is removed.
Occasionally, the tube may enter the larynx (voice box) during insertion and cause a choking feeling. When this happens, it is usually recognised immediately, and the tube is rapidly removed.
How do I prepare for High resolution oesophageal manometry and 24 hour pH study?
Please read this information leaflet carefully. If you wish, feel free to share the information with friends or family, so that they can be of help and support.
If you are requesting ambulance transport, please contact your GP practice to book this. Please tell them that your appointment is 30 minutes earlier than it is, to allow time for transport delays. Unfortunately, late arrival at the hospital may mean that there is insufficient time to carry out the procedure, resulting in its cancellation. You will also need to book transport for the following day, for removal of the pH tube (please call the department to confirm the return time on the following day for removal of the pH tube).
Please refrain from wearing make-up, and do not apply moisturiser to your face or neck. It is advised that you should wear loose fitting, separate items of clothing (for example, trousers and a top, or a skirt and top) as you will be required to pass the tube underneath your clothing.
Do not have anything to eat or drink for 4 hours before the test (although you may drink only water up until 2 hours before the test). However, if you are diabetic and this is difficult for you, please call the department for advice.
If you are on any medication for your heart, breathing problems or hormone replacement therapy, please continue to take them as usual. However, it is important that you stop taking any of the following:
Medication to stop 7 days before your appointment:
Any proton pump inhibitor, such as:
- Omeprazole (Losec®)
- Lansoprazole (Zoton®)
- Rabeprazole (Pariet®)
- Esomeprazole (Guardium® or Nexium®)
- Pantoprazole (Protium®)
Medication to stop 3 days before your appointment:
Any Histamine H2-receptor antagonist, or drugs listed here:
- Cimetidine (Tagamet®)
- Nizatidine (Axid®)
- Famotidine (Pepcid®)
- Domperidone (Motilium®)
- Metoclopramide (Maxolon®)
- Mebeverine (Colofac®)
- Alverine citrate (Spasmonal®)
- Buscopan or baclofen (Lioresal®)
Medication to stop 2 days before your appointment:
Opioid medications (including co-codamol, tramadol and codeine) may affect the test results. If you normally take an opioid medication, please do not take this for 2 days before your test (if you are able to stop it). If you take an opioid medication and have any concerns about stopping it before your test, please contact the GI Physiology department on 01482 624036 to discuss this.
If you need to stop any acid-suppressing medication prior to the test, you can use antacids such as Gaviscon Advance® from your GP or chemist. Take one dose after meals, and an extra dose at bedtime. Please do not take any antacids on the day of the test.
On the morning of the test, you can continue any other medications you normally take (that have not been stopped) with a little water.
What will happen?
You should go to the Department of GI Physiology, next to Ward 14 at Castle Hill Hospital.
You do not need to be accompanied by a family member or friend for this appointment, and they will not be able to come into the room whilst you have the procedure performed. However, there is plenty of seating in the waiting area should you wish to bring someone with you for support. Please do not bring children with you to your appointment, unless they are accompanied by another adult who can supervise them.
A member of staff from the Department of GI Physiology will explain the procedure to you on the day of your test. This is to ensure that you understand the test and any implications. You will be asked to sign a consent form if you agree to have the procedure carried out. A member of staff from the Department of GI Physiology will then start the procedure.
You cannot be put to sleep or sedated during the procedure. You will be asked to sit upright on a couch. The small probe (tube) with pressure sensors will be passed through your nose and into your stomach, while you sip and swallow water to help the tube go down easily.
Once the tube is in position, it will be secured in place with a ribbon around the tube just under your nose and around the back of your head. We will then ask you to lay down (with a pillow underneath your head). The procedure will then begin, and we will give you small measured (5 mL) sips of water to swallow approximately 10 times. After this, we will ask you to sit up and then you will eat a couple of slices of bread and margarine. If you would prefer to bring your own bread/margarine (for example, gluten free bread), please feel free to do so.
The process of placing the tube and carrying out the oesophageal manometry test takes around 20 minutes. Once this the oesophageal manometry test is completed, we will have the accurate information to correctly place the overnight 24-hour pH probe (tube). The pressure sensor tube is then removed and replaced by the much smaller 24-hour pH tube that is more comfortable. This tube will stay in place for approximately 24 hours and will be attached to a recording device that you will wear like a satchel (the recording device is slightly bigger than a smart phone).
Once the pH tube is in place, a member of the Department of GI Physiology team will explain how to use the monitoring equipment and provide instructions for returning the next day. The whole appointment will take about 60 minutes, after which you will be able to return to work or go home.
It is important that you carry out your normal activities as much as possible during the 24-hour recording period, to trigger your normal symptoms. You can eat as normal during the test, although there are some restrictions on drinks (you will only be able to drink plain water, milk or tea during the 24-hour test). You should not shower or take a bath during the 24-hour test, as it could result in damaging the monitoring equipment. Full instructions will be explained to you at your appointment (you will be asked to press buttons on the machine and complete a paper diary).
You must not take your normal anti-reflux or indigestion medication during this 24-hour period, as it will prevent accurate results. You also must not take any antacid medication you may have used in the previous week, even if you have symptoms during this 24-hour recording. If you take any anti-reflux or indigestion medication during this period, you will be required to have the 24-hour pH test repeated for an accurate result.
You will need to return to the department the following day to have the pH tube and recording equipment removed (this appointment will take no longer than 15 minutes). Once the pH tube and recording equipment is removed, you can go home or return to work as normal.
Please see the video link below showing the procedure, which you may find helpful:
What will happen afterwards?
The results of the test will need to be analysed before a diagnosis can be made. Once this is done, a report will be sent to the consultant in charge of your care. You should expect to hear from the hospital within 6-8 weeks of having the test. If you have not heard from the hospital within 6-8 weeks, please contact your consultant’s secretary by ringing the hospital switchboard and asking for your particular consultant’s secretary.
Should you require any further information or advice, please contact the Department of GI Physiology on 01482 624036.
This leaflet was produced by the Department of GI Physiology, Hull University Teaching Hospitals NHS Trust and will be reviewed in July 2026.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

