- Reference Number: HEY-613/2020
- Departments: Nutrition Support
- Last Updated: 13 June 2023
Introduction
This leaflet has been produced to give you general information about your treatment. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
What is distal feeding?
Distal feeding sometimes known as fistuloclysis, means inserting a feeding tube into your fistula / stoma and administering a liquid feed into your small bowel.
Why do I need distal feeding?
As you are unable to absorb enough nutrition from food at present, it has been recommended that distal feeding be considered. This type of feeding may allow you to absorb enough nutrition to avoid / stop parenteral nutrition and is a safer option.
Can there be any side effects?
Possible symptoms may include:
- Abdominal discomfort (this should reduce gradually as the feed rate is increased).
- Diarrhoea
These symptoms should improve over time and can be treated with medications. Please inform your medical team of any problems. Tube displacement and blockage can occasionally occur.
How do I prepare for distal feeding?
Before this type of feeding can be started you will need to have tests to assess the length and health of your bowel. This involves having pictures of the bowel taken under X-ray; these are known as contrast studies. You will have a contrast swallow test which is an X-ray test where you will be asked to swallow some colourless liquid (contrast), which then passes through your stomach and bowel and can be seen on X-ray.
What will happen?
Once you have consented for this treatment, you will need to have a feeding tube placed into your stoma / fistula. This will be done by a trained professional. The tube is held in place by a balloon filled with water. Once this is done you will be reviewed by the stoma team and a bag may be placed over the tube.
Feeding will be built up gradually. This may be done using a pump (pump feeding) of small amounts via a syringe (bolus feeding). Your dietitian will supply a feeding regimen (plan) and monitor your progress.
What happens afterwards?
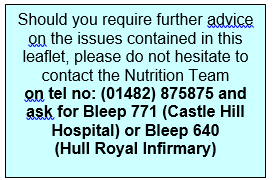
This type of feeding may be temporary or longer term. If you are to be discharged on this type of feeding, you or a family member / carer will receive training on how to give the feed and care for the tube. If you are to go home with the feed, you will be supplied with the equipment required and a list of contacts for further advice.
This leaflet was produced by the Nutrition and Dietetic Department, Hull and East Yorkshire Hospitals NHS Trust and will be reviewed in June 2025.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.