- Reference Number: HEY-957/2021
- Departments: Ophthalmology Department
- Last Updated: 1 April 2022
Introduction
This leaflet has been produced to give you general information about your condition. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is an ectropion?
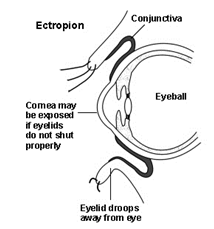
An ectropion is an outward turning of the eyelid, exposing the normally moist mucus membrane lining its inner surface, called the conjunctiva. This leads to eye dryness, soreness, redness, irritation, and in severe cases, vision problems. The lower eyelid is most commonly affected, but the upper lid can also rarely be involved.
Ectropion has many causes, the most common of which is loosening of the tissues supporting the structures of the eyelid, as a natural consequence of aging. Facial nerve paralysis (such as Bell’s Palsy) can also cause ectropion, large facial tumours can weigh the eyelid down, and scars from burns, trauma, or surgical reconstruction can contract and pull the lid away from the eye.
Our eyes need to be kept constantly wet and well-lubricated by tears. If an ectropion prevents it from closing properly, exposing the sensitive and vital clear window in front, called the cornea, the dryness can cause vision problems that may be irreversible later on.
What are the symptoms of ectropion?
Symptoms range from mild to severe, and may include any of the following:
- Eye and eyelid redness and soreness, irritation, or foreign body sensation due to dryness
- Excess reflex tearing, as the eye tries to relieve itself of the dryness
- Crusting of the eyelid margins and corners, and whitish or yellowish discharge, which may be signs of infection
- Blurring of vision, whether intermittently or constantly, from an unstable tear film, or corneal involvement
How is ectropion treated?
Conservative treatment for ectropion involves alleviation of the dryness with lubricant eye drops, and minimization of exposure by using lid-taping measures to help oppose the margin back against the eye, or keep it closed during the night.
Definitive management, however, requires surgery to address the underlying cause of the ectropion. This is usually a 30-minute day procedure done under local anaesthesia, though complex cases may take longer. If present, masses may be removed and contractures are released, then lid is tightened much like a belt against one’s waist. After numbing the area with local anaesthetic, small incisions are made around the eye, and tissues are mobilized and re-attached using dissolvable sutures.
Can there be any complications or risks?
There will be mild to moderate pain during the injection of the local anaesthetic, but this helps to ensure comfort for the rest of the procedure. Mild bleeding is expected intra-operatively, so discussion with your doctor regarding any blood problems you may have or blood-thinning medications (such as aspirin) before the surgery will help minimize this risk. Post-operative swelling and bruising may persist for up to two weeks and are usually self-limited. There is a small risk of infection, so it is important to follow post-operative instructions closely, and to apply medications consistently. Your vision should not be affected. Recurrence can happen, and this may require repeat surgery, but this circumstance is rare.
How do I prepare for the operation?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
Further information relating to what to expect when attending for lid surgery is available in the leaflet called Minor eyelid surgery.
What will happen?
Upon arrival
You will be asked to arrive at the Eye Hospital at a specific time for your surgery; this time will have been included within your appointment letter. When you arrive you will be directed to the Day Case Unit within the Eye Hospital.
Day Case Unit
Please inform the doctor or nurse practitioner if you have ever experienced a bad reaction to any anaesthetic or numbing medicine before, for example when having dental treatment. Please tell us about any tablets and medicines that you have taken in the last few weeks. In particular, we need to know about any medication such as aspirin, warfarin, or blood pressure tablets.
Priority of patients seen
We ask you to arrive at a specific time, however please be prepared to wait up to 4 hours for your procedure to commence. This is due to the departments need to prioritise our patients for the morning or afternoon surgeries.
What happens afterwards?
A gauze eye patch will be placed over your eye for a few hours up to overnight. As such, you may not drive yourself home following surgery. Instead, you should be accompanied by a friend or family member, or otherwise taken home via taxi. Transport service can also be arranged for you by our staff.
Once the local anaesthetic wears off, you may experience some mild discomfort, which can be alleviated with over-the-counter pain medications. Upon removal of the eye patch, it is common to see it stained with blood and fluid, but this is not a cause for alarm. You will be instructed on how to properly care for your wound with clean, warm water, and how to apply the antibiotic drops or ointment thereafter. Never rub your eye or pick at the stitches, as this may cause them to come loose, or result in bleeding and infection.
Arrangements for your follow-up with us will be made prior to your leaving the hospital. This is usually between 10-14 days post-op, for wound inspection and removal of stitches.
Please contact the Eye Clinic if you need any further advice on telephone (01482) 816658 or 608788 (8.30am – 5.00pm) or Out-of-Hours (01482) 604346 (Please listen to full voice message on how to access emergency out of hours service).
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Ophthalmology Department (01482) 816658 or (01482) 608788 (08:30am -5:00pm Monday – Friday)
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

