- Reference Number: HEY1025/2022
- Departments: Ophthalmology Department
- Last Updated: 1 April 2022
Introduction
This leaflet has been produced to give you general information about your condition. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
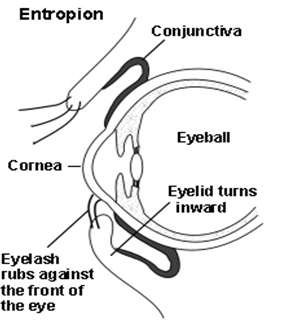
What is an Entropion?
An Entropion is a condition of the eye in which the eyelid turns inwards towards the eye. This causes the eyelashes to rub against the surface of the eye. Commonly it is the lower eyelid that is affected. Entropions mainly occur in older people when the muscles in the eyelid have become weak. If you have had a severe chemical burn to the eyes and face scarring this may also cause an Entropion to develop. In some countries Entropion is caused by an infection called Trachoma, the resulting scarring causes the lid to turn inwards.
What are the symptoms of Entropion?
You may suffer from any of the symptoms below:
- Irritation and pain on the front of the eye.
- Watering of the eye.
- If untreated, the cornea may become damaged by the development of a corneal ulcer and this could cause permanent scarring.
Why do I need treatment for an Entropion?
The usual treatment for Entropion is an operation to correct the position of the eyelid by tightening the skin and eyelid muscles. The operation is done using local anaesthetic and takes 20-30 minutes depending on the type of procedure needed. The operation is usually successful and prevents further damage to the eye caused by drying.
There are several types of surgical procedure to correct an Entropion; the surgeon will advise you on which is the most appropriate one for your eye.
While you are waiting for the operation, you may be asked to use some lubricating eye drops to protect the cornea and relieve some of the discomfort.
As a temporary measure you may be also asked to apply a tape from the lower lid to your cheek. You will be shown how to do this.
Can there be any complications or risks?
There is the slight risk of bleeding and/or infection of the wound. Any other risks which relate to your condition being treated will be discussed with you before the operation.
How do I prepare for the operation?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
Further information relating to what to expect when attending for eye-lid surgery is available in the leaflet called Minor Eyelid Surgery.
What will happen?
Upon Arrival
You will be asked to arrive at the Eye Hospital at a specific time for your surgery; this time will have been included within your appointment letter. When you arrive you will be directed to the Day Case Unit within the Eye Hospital.
Day Case Unit
Please inform the Doctor or Nurse Practitioner if you have ever experienced a bad reaction to any anaesthetic or numbing medicine before, for example when having dental treatment. Please tell us about any tablets and medicines that you have taken in the last few weeks. In particular, we need to know about any medication such as aspirin, warfarin, or blood pressure tablets.
Priority of patients seen
We ask you to arrive at a specific time, however please be prepared to wait up to 4 hours for your procedure to commence. This is because it is necessary to prioritise patients for morning or afternoon surgeries.
What happens afterwards?
Your eye will be covered with an eye pad, which will impair your vision. Because of this, you must not drive following the operation. Therefore it is advisable that a friend or a relative is asked to take you home.
The period that your eye will be covered will depend on the type of surgery that you have undergone. This period may be only a few hours or perhaps overnight but you will be advised on this after your surgery.
Once the local anaesthetic has worn off, you may experience some discomfort but this usually settles down when pain relief is taken.
Many of the operations require stitches and these are generally the type that dissolve and do not require removal. There may be occasions where your stitches have to be removed and if this is the case, before you leave the Eye Hospital a follow up appointment will be arranged for you to return for a check-up.
After the surgery, you will be advised on how to clean around your eye and when to use any eye treatments that may be prescribed, such as antibiotics, ointment or drops.
When you remove the eye pad, it is normal for it to be discoloured with blood. You should gently bathe the eyelids with cooled boiled water to remove any discharge. It is important that you do not rub your eye as you may cause some bleeding or the stitches to come loose.
You will be given an appointment to return to the Eye Clinic for the stitches to be removed and check on the eye to make sure it is healing up as expected.
Please contact the Eye Clinic if you need any further advice on telephone (01482) 816658 or 608788 (8.30 am – 5.00 pm, Monday-Friday) or Out-of-Hours (01482) 604346 (Please listen to full voice message on how to access emergency out of hours service).
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Ophthalmology Department on (01482) 816658 or (01482) 608788 (08:30-17:00 Monday-Friday)
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

