- Reference Number: HEY1020/2018
- Departments: Orthopaedics
- Last Updated: 1 February 2022
Introduction
This leaflet has been produced to give you general information about the frame treatment that has been advised by your consultant orthopaedic surgeon. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the limb reconstruction team, but may act as a starting point for discussion. If after reading this leaflet you have any concerns or require further explanation, please discuss this with a member of the Limb Reconstruction Team.
Limb Reconstruction Team
The Limb Reconstruction Team consists of consultant orthopaedic surgeons, frame specialist nurse and specialist physiotherapist.
What is a frame?
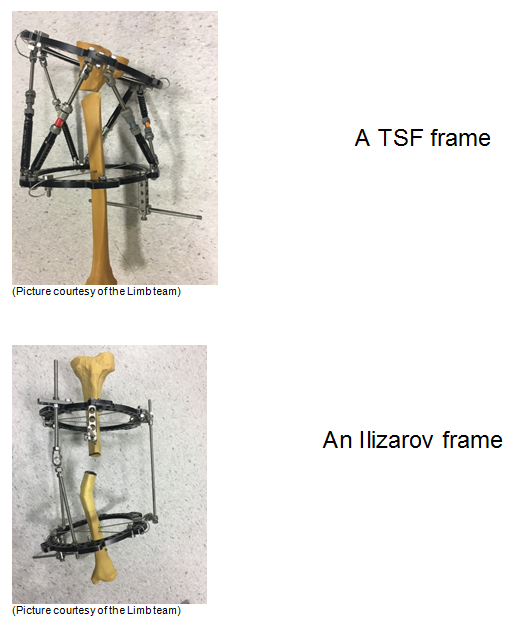
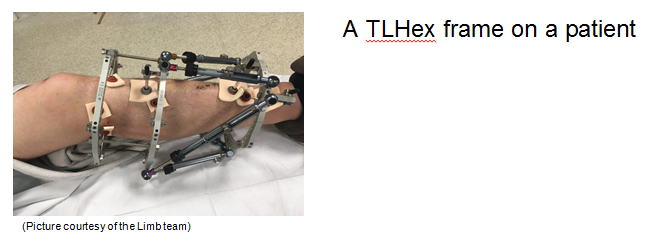
A frame is a special form of scaffolding (external frame) that can hold and control your bone to aid repair. Sometimes this is referred to as an Ilizarov frame, cage or a circular frame, because of the rings that go round the leg.
The Ilizarov frame was invented in 1951 by a Siberian doctor named Gavril Abramovich Ilizarov. His method has been used extensively in the UK since the 1990s.
More recently this method has been adapted so it is easier, with computer software, to straighten deformed or broken bones. These frames include the TSF (Taylor Spatial Frame) and TLHex (True Lok Hex).
Every frame is unique, and is made up from a wide choice of components which are connected to your bone with wires and pins. Sometimes the frame crosses the knee or foot.

Some of the different components used to make an Ilizarov frame
Why do I need a frame?
Some deformities or more complex fractures, especially those near to a joint, are better controlled and treated with circular frame.
Some patients may require a frame because other forms of treatment have failed, for example fracture non-union (where a fracture has not healed) or for osteomyelitis (bone infection).
Can there be any complications or risks?
All procedures have potential complications and risks. Frame surgery carries more risk as it is generally used for more complicated problems and injuries.
Damage to other structures
You may already have damage to nerves, blood vessels and tendons, especially if you have had a fracture. It is also possible that these structures could be damaged at the time of your surgery, when the wires and pins are inserted.
Pain
All patients with a frame will experience some pain and discomfort initially. We will provide pain relief medication to help with this. Please let us know if you are in pain.
Many patients will then be given a programme of adjustments to perform on their frame. This will be explained to you. Your discomfort might increase for the period of your adjustments, especially if you did not have a fracture but have a frame to correct a deformity or lengthen your leg. Sometimes the wire or pin has to make a new tract in the skin as the leg is straightened, this can be painful and can cause further scarring. Occasionally excess tissue formation and scarring can happen around the pin sites.
Thrombosis
Because you will not be walking as much as normal, you will have an increased risk of developing a blood clot (thrombosis) in your leg or lungs (pulmonary embolus (PE)). A thrombus is a serious complication which can cause long term problems with leg swelling, skin problems and can be fatal, although this is rare. We ask you to give yourself a daily injection of blood thinning medication until you are walking regularly again. If you run out of injections please contact your GP who will be able to prescribe some more. We will advise you when you are walking well enough to stop the injections, for some patients this is only after their frame has been removed.
Infection
All patients are at risk of having skin infections around the entry points of the wires and pins, if this occurs it is treated with a short course of antibiotics. Occasionally patients have to take a longer course of antibiotics, sometimes for the duration of their frame treatment. Very rarely the infection can affect the bone or joint; this is called osteomyelitis or septic arthritis. This often requires further surgery and a long course of antibiotics which are usually administered intravenously (into a vein).
If you are having a frame because you have an “open” fracture (one with a skin wound and soft tissue injury) there is always a higher risk that bacteria has already entered your wound, increasing your risk of infection.
Joint problems
It is very important that you attend your physiotherapy appointments, do your exercises and wear your foot splint when you are resting; this is to prevent joint contracture, stiffness or dislocations. These problems are more common in patients having multiple deformity correction or lengthening surgeries.
Delayed Union and Non-Union
There is never any guarantee that your bone will heal (unite), especially if you had an open injury. Smoking is the biggest risk factor for delayed or non-union as it delays bone and soft tissue healing. To reduce the risk of this complication we recommend that you must stop smoking. Please tell us if you need support to stop smoking.
There is some evidence that anti-inflammatory drugs like ibuprofen or diclofenac can slow bone healing, please do not use these whilst your frame is on. We would also advise you not to drink fizzy drinks as these may harm bone health.
Further surgery
Some patients require further surgery after the first frame has been put on. Sometimes this is planned from the beginning or may be required due to complications.
Following extensive assessment and advice from their consultant and a team of specialists, a very small number of patients require an amputation after their frame treatment. This could be because of prolonged time in the frame, failure of the bone to heal, pain, infection or other reasons. This is can be a very difficult decision to make and will require careful consideration and discussion with many different specialists.
Daily life
It will take you some time to adjust to the practicalities of living with the frame by making adjustments to clothing, your sleeping position and daily activities. Before you go home we will make sure you know how to look after your frame and signs of any complications that you need to look out for.
How do I prepare for the frame?
We have provided you with this information so that you can consider the procedure further. Share the information with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this treatment. This information can be very distressing to some patients and you may feel overwhelmed. You will meet with the consultant again prior to your surgery and meet the other members of the limb reconstruction team who will be happy to answer your questions. If there is anything you wish to discuss further please is contact the Ilizarov specialist nurse, their details are found at the end of the leaflet.
When the decision has been made to have the procedure you will be asked to sign a consent form. If you have a fracture your surgery is undertaken as soon as possible by one of the limb team consultants. If it is a planned, elective procedure, you will be placed on the waiting list. Also take some time to think if there are any changes you can prepare for to make your home environment easier when you return there.
What will happen?
If you are on the waiting list to have an elective operation, you will be contacted by the pre-assessment team. You will be asked to attend a pre-assessment clinic where the nurses will ask you questions about your general health and home circumstances and perform investigations including blood tests, skin swabs to check for MRSA and MSSA (to reduce your risk of infection) and an ECG (electrocardiogram) for some patients. This normally takes place in the pre-assessment clinic at Castle Hill Hospital (Hull Royal Infirmary for children). At this clinic the nurse will explain to you where to go on your day of surgery.
On the day of surgery you will be visited by the anaesthetist to discuss the type of anaesthesia and post-operative pain management.
If you have had a fracture, we usually have time to before the operation for you to see a model frame with the physiotherapists, to meet other members of the frame team and to have your questions answered. Unfortunately you may have to wait for your surgery if you are admitted at a busy time and sometimes your surgery may be postponed for emergency cases.
What happens afterwards?
After surgery you will go back to the ward to recover from your anaesthetic. The average length of stay is three days but this is dependent on the surgery, your pain and your home circumstances. On the ward the nurses will show you how to care for your pin sites, this is usually done two days post-surgery. You will be told whether you can walk on the operated leg and will have extensive physiotherapy on the ward, to ensure you are able to function as safely as possible prior to your discharge from the ward. The physiotherapist will make a foot splint to maintain your foot and ankle position, unless your frame already spans your ankle joint.
You will be given a clinic appointment to see the specialist nurse and/or consultant, and a physiotherapist appointment will be made for you to attend for physiotherapy within one week of discharge from the ward.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Ilizarov Specialist Nurse Fracture and Orthopaedic department (01482) 674378 (answer phone 24 hours, messages picked up 7 days a week)
This leaflet was produced by the Limb Reconstruction Team, Hull University Teaching Hospitals NHS Trust and will be reviewed in February 2025.
Ref: HEY1020/2022
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

