- Reference Number: HEY-1295/2022
- Departments: Orthopaedics
- Last Updated: 1 May 2022
Introduction
This leaflet has been produced to give you general information about your injury. We understand you may not have seen a clinician face to face in fracture clinic however, most of your questions should be answered by this leaflet. If after reading it, you have any concerns or require further explanation, please do not hesitate to contact the fracture clinic team. Contact details are available at the end of this leaflet.
What is a fracture of the triquetrum?
The triquetral is one of the eight small carpal bones in the hand. A triquetral fracture is often caused by a fall onto an outstretched hand. Usually a small flake of bone called an avulsion, is pulled away by the ligament the attaches to the bone.
How should it be treated?
This injury can be treated in a wrist splint for 3 weeks, this will provide the support needed for the fracture to heal and will help relieve any pain you may feel. After 3 weeks, it can be removed without requiring a further fracture clinic review.
It is really important to note that smoking will delay the healing process and so should be avoided. Talk to your GP or go to www.smokefree.nhs.uk for more information.
To manage your pain, we advise that you regularly take simple pain relief, which can be bought over the counter. If you have allergies or conditions, which prevent the use of pain-relieving or anti-inflammatory medication, please seek advice from your doctor or a pharmacist.
What should I do in the first few days?
Complete rest is not advisable. Whilst in the splint, it is important that you try to use your hand normally when doing everyday tasks like dressing and eating. As long as you are careful and it is comfortable to do so, you can remove the splint to wash yourself. Once your hand is fully dried, reapply the splint as instructed.
Arm exercises are very important; you should move your shoulder, elbow and fingers regularly to prevent stiffness at these joints. The exercises below can be performed 4 times daily.
- Support your elbow on a table with your wrist straight and fingers pointing towards the ceiling.

Bend your fingers into your palm as tightly as you can. Hold the stretch 10 seconds.
Now stretch your fingers as wide as you can. Hold the stretch for 10 seconds.
2. Remove the arm from the sling and straighten it down by your side.
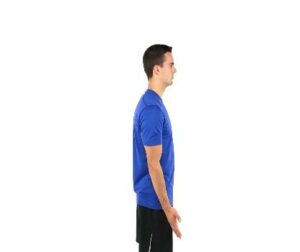

Now bend the elbow as much as possible.
Repeat 10 times slowly in each direction.
3. Bend your elbow and tuck it into your side.

Turn your palm as far as possible upwards without moving your elbow. Feel the stretch and hold for 10 seconds.
Now turn your hand back over so your palm faces downwards, feel the stretch and hold for 10 seconds.
4. Shoulder flexion

Hold a long stick in both your hands.
Allow your unaffected arm to help your affected arm lift forward and upward as high as possible.
In the early stages, you may find this easier laid down.
If you continue to have swelling in your wrist or hand, you can reduce this by sitting on a chair and placing your elbow on cushions so that it is level or slightly higher than your shoulder. In this position, point your hand towards the ceiling, open and close your fingers slowly for 10 minutes (like in exercise 1 above).
When can I start driving again?
You will not be insured to drive whilst you are in wearing a splint. It is always good to check with your insurance company however we advise it should be safe to return to driving when:
- You are no longer wearing the cast or splint
- You can comfortably grip the steering wheel, move the gear stick, pull up the hand brake and activate the indicators.
- You can perform an emergency stop.
What exercises can I do once the splint has been removed?

Hold the stretch for 10 seconds.
Now move your hand towards the ceiling. Repeat 10 times each direction.
2. Sit with your elbow tucked in by your side and your thumb upper most. Now keeping your thumb upper most move your fingers down towards the floor. Hold 10 seconds.

Next move your fingers back up towards the ceiling. Hold 10 seconds.
Movement should occur at the wrist only.
- Bend your elbow and tuck it into your side.

Turn your palm as far as possible upwards without moving your elbow. Feel the stretch and hold for 10 seconds.
Now turn your hand back over so your palm faces downwards, feel the stretch and hold for 10 seconds.
- Support your elbow on a table with your wrist straight and fingers pointing towards the ceiling.

Bend your fingers into your palm as tightly as you can. Hold the stretch 10 seconds.
Now stretch your fingers as wide as you can. Hold the stretch for 10 seconds.
This exercise you will have practiced whilst in the splint but it is important to do out of the splint as you may now gain further movement.
All photos with kind permission of ©Physiotec™
Exercises should be practiced 10 times, 3 to 4 times per day. Initially you will be stretching the muscles around the wrist that have become stiff whilst you have been in a splint. As a result, you may experience more discomfort when you start the exercises, however this is normal and does not mean you should stop. If your symptoms remain worse for more than two hours after the exercises, then you should decrease the number of each exercise that you do and build up again slowly.
After the splint has been removed when should I start increasing my activity?
Repetitive wrist and hand movements and lifting objects heavier than a cup of water should be avoided to begin with. However, as your movement improves and pain reduces, little by little you can increase the amount of weight that you are able to lift. Progressing quickly from lifting a cup of water to a heavy shopping bag for example would not be advisable, as is likely to result in overloading of the soft tissue and could consequently delay your recovery.
If you participate in an active hobby then it is advisable that you do not return to this until you have full strength and full range of movement.
If you play a sport, you can practice sports specific activities; like throwing or catching. Build up these exercises gradually from around 6 weeks, in order to help regain strength and flexibility, before returning to full training sessions and competition.
Do I require a follow up?
Do I need to be referred to Physiotherapy?
If the fracture clinic team feel you need to be seen by the Physiotherapy team, you will be directly referred to physiotherapy from fracture clinic and if this is the case, you will have been informed of this in your telephone call following your Virtual Fracture Clinic appointment. You will receive a letter or phone call to book this appointment within 2 weeks of the referral being made.
If you have not received one within this time, please contact the physiotherapy department on 01482 674880 between the hours 8.00am – 4.00pm Monday to Friday. If there is no answer please leave a message and your call will be returned with the same working day.
Most of the time however, a referral to Physiotherapy is not needed, but if you have any concerns, are unable to follow the advice in this leaflet, or if you still have reduced movement, strength or function, East Riding GP patients can contact the East Riding MSK Physiotherapy service on 01377 208300. Alternatively you can complete a self referral form on https://www.chcpmsk.org.uk/self-referral-form-introduction
Hull GP patients should call the fracture clinic number in the information below.
Do I need a Fracture Clinic follow up appointment?
A follow up appointment for fracture clinic is not required and you have been placed on a Patient Initiated Follow Up (PIFU) pathway. This means you will not have another appointment to be seen in fracture clinic.
If, however you have any problems or further queries relating to this injury within the next six weeks, you can contact us on 01482 674378 during clinic hours 9.00am – 4.30pm Monday to Friday. Please do not choose an option and when prompted leave a message if there is no answer and we will aim to get back to you within the same working day. If you have not needed to contact us in the six weeks after your injury, you will be discharged and should seek advice from your GP.
This leaflet was produced by the Orthopaedic Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in May 2025
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

