- Reference Number: HEY222-2024
- Departments: Endoscopy
- Last Updated: 1 April 2024
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should have been answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a flexible sigmoidoscopy?
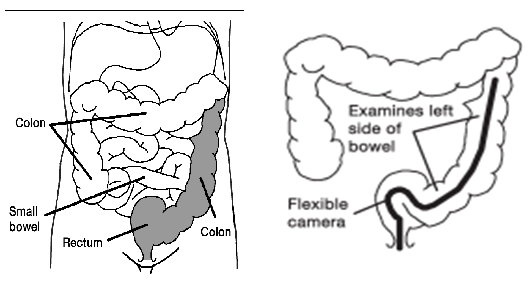
This is an examination of the lower part of your large bowel on the left side using flexible camera known as a flexible sigmoidoscope. The flexible sigmoidoscope procedure only takes about 5 to 10 minutes. It provides a lot of information for your doctor/specialist.
The patient pictures are reproduced with the permission of Health Press Limited from Neild P, Gazzard B. Patient Pictures – Gastroenterology, Oxford Health, 1997.
The shaded area indicates the usual extent of the examination.
Why has a flexible sigmoidoscopy been arranged for me?
You will have seen your doctor or specialist with concerns about your bowels, which include PR bleeding, or your bowel habit has changed and does not seem to be returning back to normal, or you might have ulcerative colitis and Crohn’s disease which requires monitoring for any changes, and evaluating bowel cancers before surgery. You may have tummy pains. Your doctor/specialist has asked for this examination as part of their investigations into the cause of your symptoms.
Do I really need a flexible sigmoidoscopy?
This examination has been arranged to look at the large bowel of the left side. It provides the opportunity to take samples of tissue called biopsies if the endoscopist thinks the bowel lining does not look normal. This does not mean there is a serious problem.
Sometimes small benign (not cancerous) growths are found during a flexible sigmoidoscopy. These are called polyps and are generally removed at the same time. We do know that some polyps, especially large ones, if left for a number of years have the potential to change into cancers.
The benefits of this examination are that it is quick, examines the part of the large bowel where most bowel problems occur and that biopsies and polyps can be removed at the same time. Most people can carry on with their day or return to work, after this examination.
It does have its limitations in that it only examines one half of the large bowel. A normal result does not necessarily mean that there is no problem with the large bowel. Therefore, this examination may be part of a series of investigations.
Are there any alternatives to a flexible sigmoidoscopy
There are X-ray examinations, which can be done. X-rays can show if the bowel looks normal or not, but they cannot always clarify what the problem is. We need to be able take biopsies and this is not possible with X-rays.
A shorter camera called a rigid sigmoidoscope can be used. In fact, you may have already had this done in the clinic. As the name suggests, it is straight and does not bend. It does see the first part of the large bowel called the rectum, but no further. Biopsies can be taken, but if polyps are found then generally further camera tests are needed to deal with them.
What if I refuse to have flexible sigmoidoscopy?
This will not alter the way we treat you and your standard of care will not change. However it will be an important piece of information about your large bowel we do not have.
Please discuss this with your doctor/specialist team.
Who will do the flexible sigmoidoscopy?
Trained and experienced nurse specialists also known as nurse endoscopists perform the majority of these examinations. Training has been provided through specialist courses. Alternatively the test may be performed by consultants or senior doctors.
This Trust is a teaching hospital and has commitments to train both doctors and nurses in all aspects of endoscopy and care. Your test may involve students training in the performance of flexible sigmoidoscopy. A senior and experienced Endoscopist supervises all students. If you do not want to have a trainee perform your procedure it will be carried out by the supervising Endoscopist.
If you have any questions or concerns about this, please discuss this before you sign your consent.
Can there be any complications or risks?
It is important to say that serious complications during sigmoidoscopy are rare.
Complication rates, that is, how often complications occur, vary across the United Kingdom. If you would like to know our rates for serious complications this can be discussed with you during your consultation.
Complications can be described as minor (mild) or major (serious):
Minor complications:
These complications are common and expected but do not last very long and do not cause serious harm.
They include feeling bloated after the examination because of trapped wind, feeling faint and dizzy, cold sweats and occasionally feeling sick. We monitor you in recovery and in the majority of patients these feelings subside very quickly (15-20 minutes) or over the next 24 hours. Over this time, bloatedness is common and comes and goes. As long as you are passing wind and going to toilet, this will settle down.
There is a small risk of bleeding from the bottom after sigmoidoscopy. The entrance to your bottom, the anus, does have a very good blood supply and this is where piles are often found. The insertion of the camera can cause a little bleeding. This should only be ‘spotting’ on the toilet paper or drops in the toilet bowl. It may take a few days for this to subside.
Major complications:
These are complications, which can be serious, may lead to admission to hospital and sometimes an operation. On rare occasions these can be life threatening, especially in people with serious and/or unstable cardiovascular or lung problems. It is important to stress major and serious complications are rare.
Complications, which can become serious and life threatening include:
- Perforation of the bowel – A small tear may be made through the bowel wall. This can especially occur in thin, diseased bowel or when polyps are been removed. If it occurs you may begin to feel unwell, feel nauseous or vomit, your tummy may become hard, swollen and painful. You may feel hot and shivery. These symptoms can occur within minutes of the perforation or may slowly develop over days.
If you have any of these symptoms YOU MUST CONTACT your doctor or the hospital Endoscopy Department or Ward 100 HRI (out of hours) as soon as possible.
- Bleeding – This can occur especially after the removal of polyps. Although great care is taken to ensure there is no sign of bleeding after a polyp is removed, the contraction of the bowel after sigmoidoscopy when getting rid of wind or when the bowels are next opened can cause the area where the polyp was to bleed. You should expect a little bleeding, such as ‘spotting’ on the toilet paper or small drops in the toilet bowl. This usually subsides as already described. If bleeding begins to increase where large clots of blood are seen and/or you begin to feel unwell or faint, please contact your doctor immediately for advice and help.
Recent evidence puts the risk of perforation between 1 in 1000 to 1 in 3000. This can sometimes be accompanied by bleeding. This can be more common with the removal of large or difficult polyps.
If polyps are removed, it is recommended that you avoid air travel, especially long haul flights, for a duration of two weeks following the procedure, particularly for large or difficult polyps.
Will I need this examination again?
For some, despite following instructions and taking the bowel preparation to empty the bowel, the view with the camera is poor. The endoscopist cannot be certain that the large bowel has been seen.
How do I prepare for the examination?
Please read all the information sent to you by the Endoscopy Department.Share the information, if you wish, with your partner and family so that they can be of help and support. There may be information they need to know.
Health questionnaire
With your appointment, a health questionnaire will be sent. Please complete this to the best of your ability. This forms an important part of assessing your ‘fitness’ for sigmoidoscopy and the potential for complications to occur, so that action can be taken to eliminate or reduce these risks.
To be able to see the lower part of the large bowel, this part will need to be free of faeces. Instructions for your bowel preparation are enclosed with this information.
If you have any special needs, disabilities or personal reasons for not being able to manage your enema please contact your Endoscopy Department so that alternative arrangements can be made.
If you have diabetes (especially taking insulin) or you have serious heart, lung or kidney problems, or concerned that a health problem you have may be affected, then contact the Endoscopy Department at the hospital where you are having your examination (see contact numbers).
Insulin – For some people with diabetes, we may need to admit them to hospital for the day and night before the test. There is a risk that the bowel preparation for the examination and restricted diet could make the control of your blood sugar difficult and make your diabetes unstable.
Latex – Please inform the department if you have a confirmed latex allergy as this will affect your appointment time.
Creutzfeldt-Jakob disease/variant Creutzfeldt-Jakob disease (CJD) – Commonly known as mad cow disease – Please inform the department if you have been notified that you are at risk of CJD/vCJD for public health reasons.
Medical devices – If you have a pacemaker or implantable cardioverter defibrillator (ICD) that has not been checked within the last six months please telephone the department as soon as possible. If the device has been checked in the last six months then all you need to do is inform the nurse on admission of the device and date last checked. Please contact the department if you have a pacemaker.
Pregnancy – It is important that you inform us if there is a possibility that you may be pregnant. Any information you share with us will be kept strictly confidential.
If your health has changed whilst waiting for this examination, please inform your Endoscopy Department.
I take tablets – do I still take then on the day?
Yes, please take all your tablets as normal. This is especially important if you have heart or chest problems.
If you take warfarin tablets, please let your Endoscopy Department know, special arrangements are sometimes needed.
CLOPIDOGREL (PLAVIX) – Please inform the department if you are taking these tablets as these may need to be stopped prior to your procedure.
IRON TABLETS – If you have been asked to take ‘picolax bowel preparation’ you must stop your iron tablets 7 days before your test.
If you take any of the following blood thinning tablets please contact the Endoscopy Department before your appointment for further advice: APIXABAN, RIVAROXABAN, DABIGATRAN, ARGATROBAN, OR EDOXABAN
What happens to me in the Endoscopy Department?
Our friendly reception staff will greet you on arrival. They will let a nurse know that you have arrived. Occasionally there may be a delay in your appointment time, due to any emergency having to take place. If there are any delays you will be notified as soon as possible and be kept informed.
A nurse will collect you from the waiting room and explain what will happen next. You will be given an approximate time of when you may be collected to go home. It is advisable to leave any valuables at home.
We will ask you questions about your general health and work through the health questionnaire you have completed for us. Please feel free to ask questions.
Due to the nature of the examination, we will ask you to undress and your belongings will be put in a hospital plastic bag and will be with you throughout your stay. A private changing area is provided. Although a gown and privacy shorts are provided, you may also wish to bring a dressing gown and slippers with you.
We will check your blood pressure, pulse, and oxygen levels, before your sigmoidoscopy.
The Endoscopist will meet you, explain the examination to you and discuss any risks or complications. You will both sign a consent form. This is to show you understand what will happen and agree to the procedure being performed. If you have any queries or worries, please tell us.
If you need glasses to read, please keep them with you at all times. Do not leave them with a relative or tucked away in a bag or pocket.
You are then taken through to the examination room. There will be a nurse or healthcare assistant in the room with you who you may not have previously met until this time. Before your sigmoidoscopy, the team in the examination room will review and confirm some details with you once more. This additional step is a safety measure to ensure that we have all the essential information about you.
Once on the examination trolley you will be asked and helped to lie on your left side with your knees tucked up as close as you can get, to your chest. This will help the camera get passed the first few bends. The Endoscopist with take images of your bowel as they go.
You can watch the examination on the TV screen if you wish. Do not hesitate to ask questions during the examination.
Following the procedure you will be taken on the trolley into the Recovery Room where you can rest on your side for a short while to enable you to pass the air that is still remaining within your colon. When you are ready you will be able to get up and dress before you are assisted to second stage recovery where you will be offered a drink before being given your discharge information.
How will I feel and will it be painful?
To help get around the bowel; air is gently passed into the bowel though special channels within the camera. To help the camera around the bowel, the endoscopist will examine your bottom first with a finger. This applies lubricating jelly (which may feel cold) to the bottom but also allows the endoscopist to feel the first few centimetres of the bowel. This part is sometimes not seen by the camera.
Air opens up the bowel so that the endoscopist can see where they are going. This will cause the bowel to stretch. You will experience a variety of feelings.
The first is usually a feeling of wanting to go to the toilet. You will be convinced you need the toilet. Please do not worry; you will not make a mess. It is just the stretching of the bowel and usually settles down as the camera travels further into the bowel.
However, bloatedness and sometimes a tightening of the tummy muscles often replace this feeling. This varies from person to person. It can catch you by surprise. Instinct tells you to hold your breath until it passes. Please try not to. Breathe normally and steadily. The feeling does not last very long and disappears once the examination is finished. Your nurse will help you.
If it gets uncomfortable let us know. We can stop; remove some air and then carry on to finish. Most people find this works and are able to tolerate the examination until it is finished.
Some people do not tolerate this test very well due to a variety of reasons. The test may be too painful. You do have the right to withdraw your consent at any time. If you wish us to stop, tell us and the examination will be stopped.
Sometimes because of the importance of the examination, the endoscopist will stop and discuss your decision with you. If you still wish not to proceed, then your wishes will be respected.
How long will the examination take?
Usually this examination takes about 5 to 10 minutes. The shape of the bowel varies from person to person and for some it can be difficult to get round. If this is the case, it may take longer.
Samples of tissue may be needed or a polyp removed, again this can prolong the examination.
When do I find out the results of my examination?
The results of the test will be provided to you as soon as your sigmoidoscopy procedure is finished including what has been found, if any biopsies/ polyps have been taken and what happens next. Sometimes further tests are needed or follow up with your specialist will be arranged.
If the examination is normal and no other investigations are needed you may be discharged back to the care of your doctor.
If you have any questions about what was found or future treatment, please do not hesitate to ask.
If biopsies and/or polyps are taken for analysis, the results of these will take up to 7 weeks. These results are usually discussed with you at your next clinic visit.
Further information
If you require further information about your test, your doctor, consultant and the Endoscopy Department is a valuable source of information.
Further information about your rights with regards to consent can be found in the following documents:
- Department of Health (2001), Guide to Consent for Examination or Treatment
- Department of Health (2001), Consent – What you have a right to expect
- A Guide for Adults. (Available from the Endoscopy Department)
- A Guide for Relatives and Carers. (Available from the Endoscopy Department)
These are free of charge.www.doh.gov.uk
Visit the Department of Health’s website at: www.doh.gov.uk and, for consent: www.doh.gov.uk/consent
Useful contact numbers:
- The Endoscopy Department, Castle Hill Hospital, tel: 01482 622069, Monday to Friday, from 8:00am to 5:00pm
- The Endoscopy Department, Hull Royal Infirmary, tel: 01482 674790 Monday to Friday, from 8:00am to 5:00pm
- Ward 100 Hull Royal Infirmary, Out of hours, tel: 01482 675100
What do the words in the leaflet mean?
- Biopsy – A sample of tissue is taken for analysis.
- Colon – This is the part of the large bowel above the rectum.
- Consent – This is the agreement between you and the endoscopist. You are agreeing to have investigations or treatment and that you understand the purpose, benefits, alternatives and risks. You and the endoscopist during this process usually sign a consent form.
- Endoscopy Department – The place where your procedure takes place
- Endoscopist – This can either be your consultant, an experienced and trained doctor or an experienced and specially trained practitioner.
- Perforation – A rare, but possible risk in which a hole or tear is made through the large bowel.
- Polyp – A common, benign (not cancer) growth arising from the lining of the large bowel. They take some years to develop. Some polyps, depending on their size and type, have the potential to turn cancerous.
- Polypectomy – The removal of a polyp usually performed at the same time as the sigmoidoscopy.
- Sigmoidoscopy – The examination of the inside of the large bowel using a long, flexible camera.
This leaflet has been written with the help, support, advice and collaboration of:
- Consultants of the Department of Gastroenterology
- Consultants of the Surgical Department
- Staff of the Endoscopy Department at Castle Hill Hospital and Hull Royal Infirmary
- Patients attending the Endoscopy Department
You will be given a Checklist to fill in and bring with you for your procedure as outlined in the link below:
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.