- Reference Number: HEY-609/2023
- Departments: Pain Medicine
- Last Updated: 28 April 2023
Introduction
This leaflet has been produced to give you general information about your treatment. Most of your questions should have been answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team who has been caring for you.
What is an epidural injection?
An epidural injection is a method of providing pain relief. It has been used for many years as an effective form of pain relief during childbirth.
An epidural is an injection into an area of your back that surrounds the spinal cord. Local anaesthetic and a steroid drug are injected. The local anaesthetic provides temporary pain relief. The steroid drug reduces inflammation to the affected area.
Epidural injections can be given anywhere along the length of the spine. This may be in the neck (cervical), ribs (thoracic), lower back (lumbar), or tailbone (caudal).
Why do I need an epidural injection?
Following your consultation with a member of the Health Care Team it was felt that this was the most appropriate treatment option for your condition.
Can there be any side effects or risks?
Although long term side effects and complications are uncommon, they can occur.
Not all nerves in the epidural space carry pain messages. Some nerves carry instructions to the leg muscles. If these nerves are numbed then your legs could temporarily become heavy or weak. You should be able to walk before leaving the department, if your legs become heavy or weak once you have been discharged, contact your GP or attend the Emergency Department, or local walk in centre/ minor injuries unit.
Also, you may be unaware of the need to pass urine; this will only be temporary, you will need to pass urine before you are discharged home.
You may have mild local tenderness at the site of the injection, which will usually settle over the next few days.
Sometimes after the procedure your blood pressure can fall and you may feel light headed.
On rare occasions during insertion of the epidural needle, the layer beneath the epidural space gets punctured. You may then get a headache.
If a severe headache does develop following your injection, take some paracetamol as directed, drink plenty of water and lay flat. If the headache continues for more than 24 hours please contact your GP or Accident and Emergency Department, or local Walk in Clinic/Minor Injuries Unit.
Other risks could include an increase in pain, infection, bruising, bleeding or nerve damage.
Advice to be read before having a pain relief procedure
The following information has been produced to ensure that you are able to have your pain relief procedure. It is essential that you read and follow the advice given below before you come to the hospital. If you do not follow this advice you may not be able to have your treatment.
Please contact the Pain Clinic if any of the following apply to you:
- You are diabetic and take medication to control your diabetes. (See below on how to manage treatment sessions booked for the morning or the afternoon)
- You have recently had an admission to hospital.
- You have tested positive for MRSA.
- You have an infection and are currently taking antibiotics.
- You think you may be pregnant.Continue your other regular medications including your pain killers except for anticoagulants (please see below.
Continue your other regular medications including your pain killers except for anticoagulants (please see below)
If you take Warfarin (Marevan), Clopidogrel (Plavix), Dipyridamole (Persantin Retard), Phenindione, Pradaxa, Xarelto, Apixaban, Sinthrome or Asasantin Retard, please notify the Pain Clinic at least 10 days before your appointment. You will need to stop taking these drugs at least 1 week prior to the procedure unless your doctor has advised against this.
If you are on new oral anticoagulant medications like dabigatran then you will be required to stop it at least 48 hrs in before the procedure.
This does not cover all blood thinning medications, please notify the Pain Clinic if you are taking any medications which thin your blood or prevent blood clots.
Depending on the reason that you need to take these drugs you may need a short course of blood thinning injections.
You may have to wait a while before your procedure, so please bring something to read or do to keep yourself occupied.
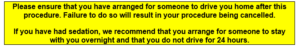
Please leave any valuables or jewellery at home. It is essential that after the procedure you arrange for an adult friend or relative to collect you by car or taxi. You will not be able to use the bus or train to travel home.
Hospital transport may be available if there is a medical need. If you think you may be eligible, then you will need to speak to your GP’s surgery who can arrange this for you.
Sometimes epidurals can be done under sedation (a drug is given to make you drowsy and relaxed but still conscious). You should not have anything to eat on the morning of your treatment, however you may have a drink (tea or coffee without milk) if you wish up to 2 hours before your appointment time.
Advice for diabetic patients only
- If you are a diabetic booked to attend treatment in the morning, you should not have your breakfast and morning diabetes medication but bring the drug with you to the clinic.
- If you are booked for treatment in the afternoon please have your breakfast and take regular medication before 7am. Thereafter only drink clear fluids (not milk) for up to 2 hours before the procedure. Please inform the clinic staff as soon as you arrive that you are diabetic, the staff will then assess your diabetes and if necessary take appropriate action to monitor and control your blood sugar levels while you are in our care.
What happens before the procedure?
You will be admitted by the nursing staff who will ask you for and record information about you. Your blood pressure will be checked and you will be given a gown to put on. The doctor will explain the procedure and ask you to sign a consent form. Please make sure you have understood what has been said and feel free to ask any questions.
What to expect during the procedure
As a precautionary measure, a thin plastic tube (cannula) may be inserted into a vein in your arm/hand.
After cleaning your back with antiseptic solution, local anaesthetic will be injected into your skin to numb it. Under x-ray screening a fine needle is introduced into your back towards the area to be treated. Once the optimal position is obtained, local anaesthetic with steroid will be injected.
- When the epidural injection takes place you may feel a pushing sensation or some discomfort.
- Contrast (a solution which shows up under x-ray) may be injected to make sure that the needle is in the correct position.
- A cold spray may be used over the injection site once the procedure is completed or a small dressing may be applied over the procedure site.
What happens after the procedure?
You will be taken on the trolley to the recovery area where the nurse will check your blood pressure and pulse. You will be asked to lay flat for approx 30 minutes and then will be given assistance to sit up.
You will be offered some light refreshment
You will be asked to rest for about an hour. After that you will be able to get up, but please check with the nurse before you do so.
You should be able to demonstrate that you are able to walk and pass urine before discharge.
What to expect afterwards
Some rapid relief of your pain may be noticed due to the local anaesthetic. It could take several days or weeks before the steroid becomes effective.
Take your regular pain killers as normal.
Try to keep on the move about the house but do not do anything too strenuous.
As your pain decreases you should try to gently increase your exercise. Simple activities like a daily walk, using an exercise bike or swimming on your back will help to improve your muscle tone and strengthen your back. The best way is to increase your activity slowly.
Try not to overdo things on a good day as this may result in you experiencing more pain the following day.
How long will the pain relief last?
This is highly variable between the individuals. Some might notice immediate pain relief; with many patients the pain initially becomes worse. Pain relief may take a number of weeks to be effective. However, pain relief may last from a few days to several months. Some patients do not get any pain relief from an epidural.
Follow up
A letter will be sent to your GP informing them of the procedure you have had, and you will be reviewed either by telephone or seen at the Pain clinic in due course.
At this review you will be asked to discuss the Pain Diary you were given at your injection appointment, please have this completed diary to hand at the time of the phone call.
Points to remember
- You will need to have arranged for someone to drive you home after this procedure.
- Please bring your glasses if you need them for reading.
- Always bring a list of all current medication.
- Continue taking all your usual medication on treatment day.
- If there is any possibility you may be pregnant please inform the doctor or nurse.
Additional information
The information in this leaflet is not intended to replace the advice given to you by your doctor or the pain service looking after you. If you require more information or have any questions, please speak to your doctor or the Chronic Pain services who are looking after you.
After the procedure if you experience unusual symptoms such as a severe headache, incontinence of urine or bowels, marked increase in pain around an injection site, fever, severe headache, new symptoms of pins and needles, new muscle weakness in your arms and legs, or you are very concerned about how you feel after the procedure, please contact your GP.
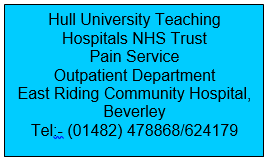
In the event of an emergency and outside normal working hours
of the pain clinic (9am – 4pm) please contact your own GP
or go to Hospital A &E, or Local Walk In Centre/Minor Injuries Unit
This leaflet was produced by the Centre for Pain Medicine, Castle Hill Hospital Hull University Teaching Hospitals NHS Trusts and will be reviewed in April 2026
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.