- Reference Number: HEY-113/2023
- Departments: Endoscopy
- Last Updated: 1 May 2023
Introduction
This leaflet has been produced to give you general information about your treatment and procedure. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a Polyp?
The lining of the bowel is made of cells that are constantly being renewed. Sometimes these cells grow too quickly, forming a clump of cells known as a bowel polyp (sometimes known as an adenoma). Polyps are not bowel cancers (they are usually benign), but they can change into a malignant cancer over a number of years.
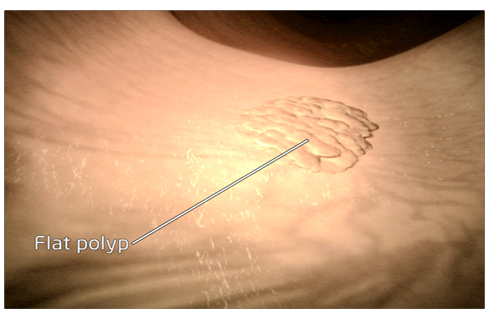
Polyps can either be flat or on a stalk. Your recent investigation has found a large polyp, which is flat, has no stalk and spreads along the surface of the bowel wall lining. We call this a ‘sessile’ polyp. To see if this polyp is benign and does not contain any cancer cells, we have recommended its removal. Because it is sessile, we need to remove the polyp using a method called EndoMucosal Resection or EMR.
What is an Endoscopic Mucosal Resection (EMR)?
An Endoscopic Mucosal Resection, sometimes called an EMR is a method used to remove larger and flatter polyps in the bowel.
A thin flexible tube called a colonoscope is guided along the bowel to find the polyp seen during your previous test.
Carbon dioxide or air is gently pumped in to the bowel through the colonoscope to allow good views of the polyp during its removal.
Blue dye may be sprayed onto the polyp to help outline the edges of the polyp to assist complete removal.
A small amount of fluid is injected under the polyp to lift it away from the deeper muscle layers of the bowel wall.
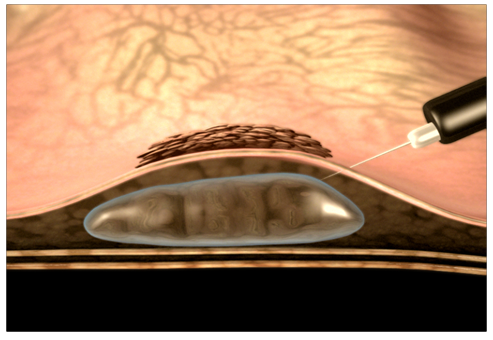
This helps to identify polyps that can be removed in this way. It also increases the chance of complete removal and reduces the risk of complications.
A wire loop is then passed down the colonoscope and over the polyp, which then can be removed. Diathermy (a low electrical current) is used to remove the polyp and seal the area left behind.

Images reproduced with kind permission from Remedica Medical Education and Publishing, London
Sometimes we inject a small amount of ink to identify the site where we have removed the polyp. This is called a tattoo.
If the polyp is greater than 2cm it may be removed in stages involving more than one procedure to reduce the risk of complications. The polyp is collected and sent for examination under the microscope
Why do we think the polyp is suitable for removal by the endoscopic technique?
The polyp we have found is flat and the samples taken from the polyp during your previous test have not detected any cancer cells at this stage, however once removed polyps are fully examined under the microscope. This type of polyp is suitable for Endoscopic Mucosal Resection and avoids undergoing a major operation.
Are there other ways of dealing with my polyp?
Yes there are other options:
Do nothing
Leave the polyp where it is. However if left, some polyps can change to bowel cancer, especially larger ones and we would advise removal of the polyp. We need to look at the polyp under a microscope.
An operation to remove the polyp
Although this is usually straightforward it does carry the risks of surgery which include infection, anaesthetic, leakage at the operation site, abdominal scars and possible stoma (a stoma is formed by part of the bowel being fixed outside the tummy and requires a bag to be worn).
How do I prepare for the Endoscopic Mucosal Resection?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
The Screening Consultant or Specialist Screening Practitioner will have discussed the procedure with you, however if there are any changes to your health or medications prior to your appointment please let us know.
The type of endoscopy you have will depend on where the polyp is located in the bowel. A flexi-sigmoidoscopy is used when a polyp has been found on the left side of the bowel and a colonoscopy is used when a polyp has been found on the right side of the bowel. Please read the procedure information provided and do not hesitate to contact us if you have any questions.
You will also be asked to take a bowel preparation to clean the bowel again as it is very important to be able to see the polyp clearly during removal. Please read and follow the instructions carefully. We cannot stress enough that you must take the bowel cleansing medication as directed and drink plenty of water in between.
Do not drink any fluids two hours before your procedure.
What will happen?
The Endoscopic Mucosal Resection will be carried out by a Screening Colonoscopist on the Endoscopy Unit at Castle Hill Hospital or Hull Royal Infirmary.
The nursing staff will greet and support you throughout your stay. You will be asked to change in to a gown and have your blood pressure, pulse and oxygen levels checked. A needle will be placed in a vein on the back of your hand or in your arm so that we can provide you with sedation and pain relief.
The Screening Colonoscopist will explain what is going to happen, answer any further questions and ask you to sign a consent form.
You will be asked to lie on your left side on the examination trolley although your position may change during the procedure. The nurse will monitor your pulse and oxygen levels throughout the procedure. You will also be given oxygen by a nasal tube.
The carbon dioxide or air can make you feel bloated and uncomfortable during the procedure so please let us know how you are feeling.
Endoscopic Mucosal Resection may take longer than your previous endoscopic examination.
What happens afterwards?
After the procedure the endoscopy staff will move you into the recovery area where your recovery will monitored. This will involve checking your blood pressure and pulse at regular intervals. You will be asked to stay on your side and get rid of any wind as you may feel bloated.
As you continue to recover you will be sat up and eventually you will be able to get up and have a drink.
Please take care. Initially you may feel dizzy and a little disorientated when getting off the examination trolley.
If you live alone or you do not have anyone who can be with you, please contact your Bowel Cancer Screening Centre so that other arrangements can be made.
We will be able to discuss your test results with you before you go home but samples may have been taken and these results may not be available for a few weeks. Your GP will receive a copy of the endoscopy report.
We would advise against travelling abroad within 2 weeks of an Endoscopic Mucosal Resection. If you have any travel plans please discuss these with us.
Do I really need someone with me after a colonoscopy?
Yes, this is very important. The sedation given can have effects, which last some 24 hours after the colonoscopy. You can become forgetful and also sleepy again.
Your test may be cancelled if you do not arrange to have someone to collect you and stay with you for the next 24 hours.
We strongly recommend that for the next 24 hours you:
- Do not drive
- Do not return to work or operate machinery
- Do not sign any important/or legal documents
- Are not left alone, you may be at risk of injuring yourself
- Are not left alone to care for children
You will be provided with an advice sheet before you go home which does include information on what to look out for and who to contact if you have any problems or concerns.
A Specialist Screening Practitioner from the screening centre will ring you at home a day or two after your procedure.
Are there any risks and possible complications?
There are some risks and possible complications associated with Endoscopic Mucosal Resection. Risks mean complications may occur.
The risks for Endoscopic Mucosal Resection are higher for bleeding and perforation than a standard removal of polyp.
Minor Complications
- Bloating can occur after the procedure with trapped wind, feeling faint and dizzy, cold sweats and occasionally feeling sick. This usually subsides very quickly, although feeling bloated may come and go over the next couple of days this will eventually settle.
- Bleeding can occur from the bottom (the anus) which has a very good blood supply and is the area is where piles (haemorrhoids) are found. Inserting the scope into the bottom can cause this type of bleeding which may be spotting on the toilet paper or drops in the toilet which should settle in a day or two.
- Blue or black dye may be seen next time you go to the toilet if used during the procedure
Major complications
The standard removal of a polyp can cause heavy bleeding or perforation. It is estimated that heavy bleeding could happen in around 1 in every 250 colonoscopies and the chances of a perforation happening are about 1 in 1,000.
The level of risk depends on how big the polyp is and where it is. There are no national figures we can provide for Endoscopic Mucosal Resection, but estimates are made through current endoscopy research (see below). If you would like to know our rates for serious complications please ask and we will do our best to answer your questions.
- Heavy bleeding can happen in around 1 in every 50 colonoscopies. It can happen at the time but can also present a few weeks after the procedure. Bleeding usually stops on its own but occasionally it may require a hospital stay, blood transfusion or further treatment. When you have had a polyp removed you should expect a little bleeding such as ‘spotting’ on the toilet paper or small drops in the toilet bowl. This usually subsides quickly. If bleeding begins to increase or large clots are seen and you begin to feel unwell or faint you must seek medical advice.
- Perforation (making a small hole in the bowel wall) the chances of this happening are about 1 in 100. It can occur at the time but can also occur a few weeks after the test. If this happens you may need an operation to repair your bowel. As with any bowel surgery this carries the risk of a stoma. If you develop any of the following symptoms seek medical advice immediately:
-
- You feel unwell or hot and shivery
- You feel nauseous or vomit
- Your tummy becomes hard, swollen and painful
- Sedation is usually a combination of pain relief medication and a sedative, both of which can have an effect on the heart and lungs. Some people can be particularly sensitive to these drugs and can breathe too shallow and slow. If this happened we would stop the test and give antidotes to the drugs to reverse their effects. In some people with serious heart or lung problems these drugs can cause a person to stop breathing or the heart to stop beating. This is a very rare but serious complication which needs resuscitation and admission to hospital. If such a situation developed it may be fatal.
Other risks
- Incomplete removal or unable to remove the polyp. If this happens it may mean you have to come back for further procedures or the polyp may have to be removed in a different way. We will discuss this with you before you go home
What happens if the polyp will not lift when injected?
If the polyp will not lift when injected this tells us that we cannot remove it using this technique. If this happens, we may take some more samples and refer your care to another consultant to explore another way to remove it. We will talk to you about this before you leave the department.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact us at Bowel Cancer Screening Centre at Castle Hill Hospital, Tel: 01482624139.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

