- Reference Number: HEY-1401-2023
- Departments: Gynaecology
- Last Updated: 30 November 2023
Introduction about Early Medical Abortion (EMA)
Early Medical Abortion is a medical treatment that involves taking oral and vaginal medication to cause an abortion in a pregnancy gestation that is less than 9 weeks and 6 days.
Although this document refers to the term woman/women, it is applicable to anyone that can become pregnant regardless of whether you identify as a woman or not.
Where will I take my medication?
You have the choice of having the medication in the hospital clinic or you will be provided with the medication to take at home.
Are there any risks with this type of treatment?
Problems (risks) at the time of the abortion are not very common. The main risks are:
- Excessive bleeding (less than 1 in 1000 risk in early abortions). This may require a blood transfusion.
- Failure of the abortion and continuing pregnancy (less than 1 in 100 risk in early abortions). This may require further treatment.
Are there any risks after the abortion?
You are more likely to get problems after an abortion. Again these problems are not common. The main risks are:
- Retained tissue (approximately 3-6 in 100 risk, dependent upon gestation). This may require further treatment.
- Infection of the uterus (up to 1 in 10 risk). This is usually due to a pre-existing infection.
You will also be offered screening before the treatment. If an infection is not detected or remains untreated it may become severe, causing Pelvic Inflammatory Disease (PID).
- Some women may experience short term emotional distress after an abortion. There is a slight increased risk to mental health disorders after an abortion compared with childbirth, but no evidence that these problems are actually caused by the abortion. They are often a continuation of problems experienced before the abortion.
- There is no proven evidence that having an abortion will cause a future ectopic pregnancy or infertility.
Abortion methods using Mifepristone and Misoprostol may not be suitable for you if you have any of the conditions below:
- High blood pressure not managed by medication.
- High cholesterol.
- On long term cortico-steroid treatment.
- On long term anti-coagulant treatment.
Please inform the nurse or doctor as they may need to discuss this further with medical colleagues at the hospital.
Will I have any side effects from the drugs?
You may get some of the following side effects. Once the treatment has worked these side effects usually stop.
- Nausea 40 in 100 women
- Vomiting 20 in 100 women
- Diarrhoea 15 in 100 women
- Headache 16 in 100 women
- Dizziness 25 in 100 women
- Flushes/sweats 25 in 100 women
What happens if I take the medication at home?
If you choose to take all of the medication at home you will only have to visit the hospital clinic once at your initial consultation.
You will have a consultation and full medical assessment with a Clinical Nurse Specialist (CNS) in the Pregnancy Advisory Service (PAS) to assess your suitability for treatment.
You will be offered a full sexual health screening when you attend clinic. Antibiotics will be provided if required and follow up will be requested via the Health Advising team at Conifer House.
You will be supplied a pack of medications containing the Misoprostol and Mifepristone that you will need for the medical termination at home, and this will include a leaflet detailing how and when you take the medication.
You may also be given/supplied your chosen contraceptive method. This will depend on what you have decided to use following the abortion. The nursing staff will discuss this with you. If you are wanting to use the Combined Oral Contraceptive Pill (COCP) or the Progesterone Only Pill (POP) as contraception then the nurse will advise you when to start taking your pill.
You will need an adult who is aware of your treatment to stay with you at home on the day that you have the Misoprostol tablets and until you think the abortion is complete. This will usually be 5 to 6 hours after having the Misoprostol tablets; however, sometimes it may be quicker or take longer. Please ensure you have a supply of pain relief at home. A hot water bottle is also useful for the relief of period type pains.
You can carry on with your normal work and home life. You may experience some vaginal bleeding and period type pains cramps. You can take simple pain relief such as Paracetamol and Ibuprofen. It is unlikely that the abortion itself will happen after the first tablet. However, some women will experience vaginal bleeding and actually pass the pregnancy. If you are worried you should contact the clinic or the emergency contact telephone numbers below.
How do I take my medication at home?
Instructions for using Mifepristone (First medication)
- Mifepristone 200mg (1 tablet) to be swallowed with a glass of water.
Instructions for using Misoprostol (Second medication)
- You will use 6 misoprostol tablets in total.
- Use the first 4 tablets by either placing them into your vagina or in your mouth between your cheek and gum (please see diagrams below).
- Then 3 to 4 hours later use the remaining 2 tablets in your vagina OR between your cheek and gum.
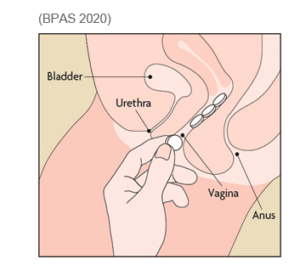
Into the vagina
- Insert 4 tablets as high as possible in the vagina. The exact position of the tablets is not important provided they do not fall out. You can put the tablets in while lying down, squatting, or standing with one leg up – whatever is most comfortable.
- Insert the 2 remaining tablets 3 to 4 hours later if there is no evidence that you have passed the pregnancy vaginally.
OR
Into the mouth between cheek and gum
- Place 4 tablets into the mouth between the upper cheek and gum (2 on each side) and allow the tablets to dissolve for 30 minutes. If the tablets have not completely dissolved within 30 minutes, you may swallow what is left with water.
- Repeat with the remaining 2 tablets 3 to 4 hours later if there is no evidence that you have aborted the pregnancy
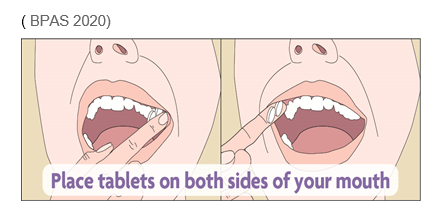
Some clients describe the taste of misoprostol as unpleasant and the texture chalky. Placing the tablets between the cheek and gum is associated with higher rates of nausea, vomiting and diarrhoea.
What will happen next?
Once you start to experience vaginal bleeding (usually a couple of hours after having the Misoprostol tablets), you may see large blood clots or pregnancy tissue. The pregnancy tissue will be larger and more recognisable at higher gestations. Under 8 weeks, you are only likely to see the pregnancy sac which is where the early pregnancy develops. If you are closer to 10 weeks pregnant the fetus is about 3cm long (the size of a large grape) and you may recognise its shape. If you are worried about what you may see then please discuss this with the nurse in the clinic.
Most women pass the pregnancy within 4 to 5 hours after taking the Misoprostol tablets. For others it can be quicker or take longer. Once the pregnancy passes, the amount of vaginal bleeding should noticeably reduce.
Once you have passed the pregnancy the vaginal bleeding should start to slow down and the pain should start to go away. You may find it comfortable to lie down, but some women will feel more comfortable walking around, or sitting down watching TV. It is up to you and how you feel. You can use your toilet as often as you like and flush it as normal.
If you have not started to experience vaginal bleeding within 24 hours of taking the Misoprostol tablets contact the clinic on the contact telephone numbers below for advice.
You should not have any leftover tablets – but if you do, please do not throw them away, please return them to GOPD or take them to a local pharmacy or GP surgery for safe disposal. Leftover Misoprostol tablets are not sufficient to cause an abortion and it would be illegal to use them for this purpose. If you think you have a new or continuing pregnancy following your treatment, you should telephone for further advice.
Will I have any pain?
Most women have some period type pains/cramps during and immediately following the treatment. In some instances this can be intense. Usually this intense pain does not last for long. Once the pregnancy passes, the amount of pain experienced should noticeably reduce. In a few women the period type pain may last for approximately 5 days after the abortion. The pain/cramps should be relieved by taking simple pain relief tablets such as Paracetamol or Ibuprofen.
How long will I bleed for after the treatment?
You may experience vaginal bleeding for 2 to 3 weeks following the treatment. However, some women bleed less than this, while others may bleed up until their next period. If you are using tampons, please change them regularly to reduce the risk of infection.
Do I need to have a follow-up appointment?
No. A nurse from the ward will contact you 72 hours after treatment on your given telephone number to check that you are okay. Please ensure that you have your phone to hand and switched on if it is a mobile phone. The phone call will appear as blocked or withheld. We are able to leave a voice message but are unable to send a text message.
If we have not contacted you on these days then please contact the clinic on 01482 607829.
You will be given a low sensitivity urine pregnancy test (LSUPT) to use 3 weeks after you have had your treatment. This pregnancy test only registers pregnancy hormone levels greater than 1000 iu/L (most normal UPT register pregnancy hormones at 25 iu/L). This pregnancy test is only to be used to confirm the abortion.
You will be required to sign a Patient Advice Leaflet before leaving the clinic and the medication is supplied to confirm you understand when the pregnancy test is due and the importance of contacting the Pregnancy Advisory Service if the pregnancy test result is positive.
Is there anything I should look out for when I go home?
You should contact the Women and Children’s Hospital on the contact numbers below or your GP if any of the following apply to you:
- You have severe pain which is not relieved with simple pain relief tablets.
- You feel feverish.
- You have excessive vaginal bleeding.
- You have an offensive vaginal discharge.
- Your period is later than expected and you still feel pregnant.
Sepsis can be caused by an infection and whilst it is rare, it can be serious especially if it is not detected. Symptoms of sepsis can be like having the flu at first. If you have any of the signs below it is important to seek urgent medical advice:
- Confusion
- Slurred speech
- Extreme shivering
- Severe muscle pain
- Being unable to urinate
- Severe breathlessness
- Cold, clammy and pale or blotchy skin
Who can I contact if I have any questions?
If you have any concerns or need further information then please do not hesitate to contact:
- Gynaecology Pregnancy Advisory Service clinic (8am to 6pm Monday to Friday) – 01482 607829
- Cedar Ward (6pm to 8am Monday to Sunday) 01482 604387
- Early Pregnancy Assessment Unit – EPAU (8am to 3pm Saturday and Sunday) 01482 608767
- If you require any counselling support please self-refer on the following number: – Temenos Psychotherapy & Counselling 01482 844038
- For contraception information please use the following website: http://www.fpa.org/uk/
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.
