- Reference Number: HEY-508/2023
- Departments: Day Surgery (DSU), Plastic Surgery
- Last Updated: 10 January 2023
Introduction
This leaflet has been produced to give you general information about your discharge. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
What should I do following discharge?
Following your discharge, please take the following advice.
- Take plenty of rest at home over the next few days.
- Do not allow your injured hand to hang down as this may cause pain, swelling or bleeding.
- Place your arm on two or three pillows at night in bed or when sitting in an armchair during the day.
- Wear the sling as instructed.
- Exercise your shoulder and elbow to prevent stiffness.
- Do not try to use your injured hand
- Your dressing and plaster cast should be kept clean, dry and undisturbed.
Can there be any complications or risks?
The tendon(s) that have been repaired are very fragile and can be easily damaged following surgery.
Do not attempt to move or exercise your fingers until you have been advised at your first outpatient appointment. It is extremely important that you do not remove the plaster cast as it is there to protect the tendon repair. If the cast becomes loose, broken or uncomfortable, call the Plastics Trauma Team so that it can be repaired or replaced as soon as possible.
What follow up care will I need?
You will receive an appointment to attend the Plastic Surgery outpatient department to see the doctor, nurse or physiotherapist for a wound review. The plaster cast is usually replaced with a lightweight plastic splint at this time.
What pain relief should I take?
It is advisable to have a supply of mild painkillers at home, which should be used as directed on the packet if you have pain. If you have any bleeding (other than mild oozing), or your fingers swell, turn red, white or blue, you should contact the Plastics Trauma Team for advice.
When can I return to work?
Your doctor or physiotherapist will advise you about returning to work after your operation.
When can I drive?
You should avoid driving until a doctor or physiotherapist advises that it is safe. It is wise to inform your insurance company about your injury to confirm that your insurance remains valid.
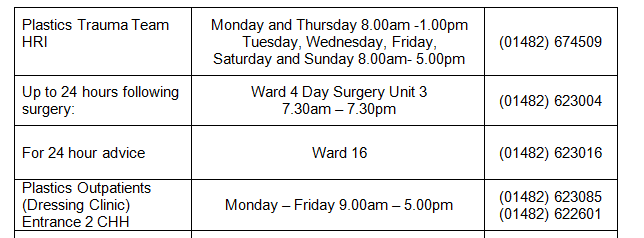
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact any of the following.
Please contact the area where you had surgery in the 1st instance if the area is open.
General Advice
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, your information will be shared between members of the healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health or social organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You. www.hey.nhs.uk/privacy/data-protection
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.
This leaflet was produced by the Plastic Surgery Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in January 2026.
Ref: HEY508/2023

