- Reference Number: HEY-727/2023
- Departments: Plastic Surgery
- Last Updated: 1 March 2023
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
Rest
When you go home it is important that you take plenty of rest. You will need someone else to do the housework. You should avoid strenuous activities, exercise, excessive stretching or heavy lifting (including lifting children) for at least six weeks.
You should not drive until at least after your outpatient appointment, and you should make sure that you are fit enough to do an emergency stop.
You can now start to use your arm more freely, try not to keep your arm stiff.
Your consultant asks that you wear a good supportive, non-wired bra, day and night for six weeks after your operation, as this will help to shape and support your new breast. It is advisable to avoid under-wired bras for at least a year after your operation unless you have been given different instructions by your consultant.
Dressings
Dressings should be kept clean, dry and undisturbed.
Do not use any perfumed products i.e. sprays or creams near your wound as these may irritate it. If you have any bleeding (other than oozing), swelling, redness or discharge you should contact the ward for advice.
Follow Up
Your consultant will usually use internal stitches, which do not need removing. They will dissolve within about 10 weeks. Occasionally sutures that need to be removed are used. It is not a painful procedure to have them removed. This will usually occur 10-14 days after surgery. Following the removal of your stitches your new breast will still be quite swollen.
Pain Relief
It is advisable to have a supply of mild pain relief at home, which should be used as directed on the packet if you have pain. We recommend that you take paracetamol based pain relief and avoid ones that contain aspirin.
Sun Care
You should protect your scars from the sun for the first twelve months by using sun block or clothing. Until the scars are fully matured, they will burn very easily.
Period of Recovery
We advise that you have about six weeks off work to recover after your operation, however if your job is quite physical or involves a lot of heavy lifting, you may need to take longer. Your consultant will advise you at your outpatient appointment. You can submit a self-certification certificate for the first week, after this you will need to get a sickness certificate from your GP (General Practitioner) or the doctor on the ward. There is no reason you cannot begin swimming or taking other exercise once your scars are healed, although you should check with your consultant first. This is typically 8-12 weeks following your surgery. You can also resume normal sexual relationships at this point although your new breast will probably still feel quite tender, and may not have a normal sensation.
The usual amount of time between your first operation and the second operation to make your new nipple and reshape your other breast (if you requested this) is at least three months. The reconstruction of your nipple and areola (the area around the nipple) is a relatively small procedure and can sometimes be done under local anaesthetic.
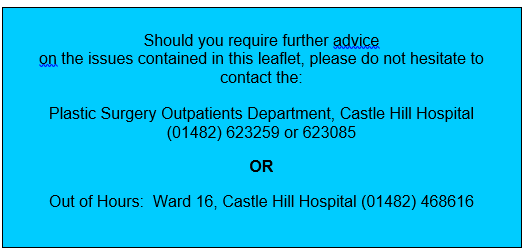
If you have any problems with your wounds please contact the Plastic Surgery Outpatients Clinic on (01482) 623259 (Mon-Fri 8.30-4.30) or Ward 16 on (01482) 468616 (out of hours).
This leaflet was produced by the Plastic Surgery Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in March 2026.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

