- Reference Number: HEY-372/2016
- Departments: Diabetes
- Last Updated: 1 June 2016
Introduction
This leaflet has been produced to give you general information about Diabetic Charcot foot. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your healthcare professional, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
What is a diabetic Charcot foot?
Charcot foot (Charcot arthropathy) is a serious condition that can affect the feet of people with diabetes. Diabetic Charcot foot occurs in people who have neuropathy (loss of sensation). An injury happens which causes the bones in the foot to either break or dislocate. The injury can happen without any knowledge to the patient. The symptoms that occur include swelling, heat, and occasionally some redness to the foot. Some patients experience some pain whilst some patients experience no pain at all.
Charcot foot is more likely to happen if you:
- Have had diabetes for a long time.
- Have nerve damage to your feet (diabetic neuropathy).
- Injure your foot.
- Have a good blood supply to the feet.
- Have an existing foot ulceration.
Can there be any complications or risks?
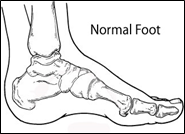
Charcot foot can cause changes in the shape of the foot which can happen very rapidly and can take a very long time to heal. Once your foot has changed shape it will not return to normal.
If you have nerve damage in your feet you may not feel any pain from the damage and may continue to walk on your foot without realising there is a problem.
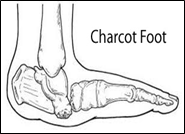
Charcot foot needs immediate treatment. Any delay may mean that any change in the shape of your foot is much worse. Treatment aims to reduce any foot shape changes as these can lead to severe deformity, foot ulcers, disability and on occasion amputation of the foot.
If the affected foot changes shape it will mean it will be difficult for you to get shoes to fit properly. You may need to see the orthoptist for specialist shoes and insoles to be provided as well as continue to see the podiatrist regularly to prevent your foot from developing any other complications.
Will I need specialist tests?
As Charcot foot will usually make the affected foot swollen and hotter. The temperature of both feet will be taken to see if there is a difference. An X-ray of the foot will be taken to see if there is a break or dislocation and how much damage has been done. It will be necessary to repeat the temperature tests and X-rays whilst you are having treatment to see if the foot is healing.
How is it treated?
The length of time it takes for Charcot foot to heal will vary from person to person but usually goes through three phases:
Active phase: 0-3 months (acute, development-fragmentation).
- Treatment must start as soon as possible.
- The foot must be immobilised in a plaster cast or walking brace to try and prevent changes in shape.
- Weight must be kept off the foot so you may need to use crutches or a wheelchair. Walking on the foot may delay healing and increase the chance of deformity.
Healing phase: 4-8 months (sub-acute, coalescence).
- The bones are starting to heal and fuse back together.
- Some weight can be put on the foot.
- The foot must remain in the plaster cast or walking brace.
Rehabilitation: 8 month+ (chronic, reconstruction-consolidation).
- The bones have become strong. The amount of weight put on the foot can be increased slowly.
- The foot must be protected by using special insoles and shoes that support the foot and allow for any changes that have occurred in the shape of the foot.
- If there is a large change in shape then surgery may be necessary; including the possibility of amputation.
What can I do to help prevent it?
- Keep blood glucose under control.
- Check your feet every day for signs of damage or injury.
- Be careful to avoid injury to the foot from knocks and trips/falls or from making drastic changes in your activity level.
Remember – If you notice any change to your foot such as swelling, redness, heat, increase in pain or change in shape contact your podiatrist, GP or nurse immediately.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact:
Diabetes Foot Protection Team,
The Diabetes Centre,
Brocklehurst Building,
Anlaby Road,
Hull, HU3 2RW.
Telephone number: (01482) 675345 Monday to Friday 8:30am to 5pm.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

