- Reference Number: HEY1178/2020
- Departments: Emergency Department, Paediatrics
- Last Updated: 16 November 2020
Introduction
This leaflet has been produced to give you general information about your child’s condition. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team caring for your child but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for your child.
Concussion
Concussion can result from a minor head injury and can cause a range of symptoms in the time after injury. It is not linked to a particular problem within the brain, but rather as a result of the injury itself.
After head injury your child may have:
- Persistent headaches, nausea, dizziness
- Difficulty concentrating or being involved in an activity for a longer time period
- Change in personality, for example being more irritable or angry in the period after having a head injury
- Vision problems (focusing/blurring of vision)
- Being more sleepy or tired than normal
The symptoms can come and go for a few weeks, but, importantly, the symptoms will improve with time and rest in most cases. More information can be found at:


What can I do to help my child?
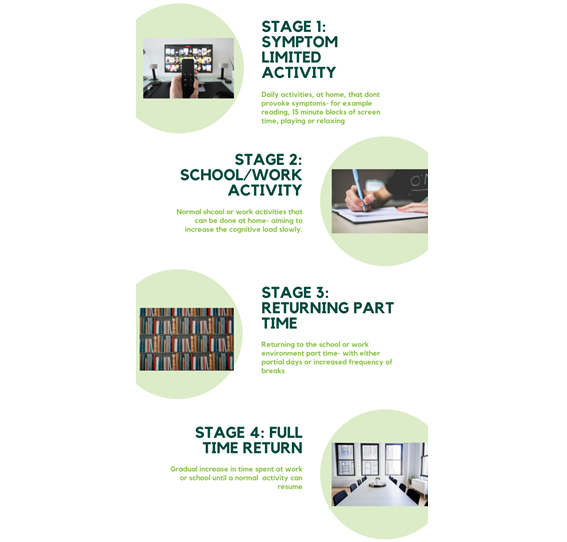
Try to encourage gradual return to normal rather than jumping straight back into activity. This is important as it allows the brain to rest and recover from the injury it has had. We advise 24 – 48hours of rest (including no screens, avoid small print reading and avoid bright lights and loud noises ) after a head injury that causes symptoms, followed by gradually increasing normal activity:
- STEP 1: Start with activities that do not cause symptoms (headache / vision problems/ nausea), for example 15 – 20 minute blocks of reading, screen time, playing. If symptoms come back, rest.
- STEP 2: Normal school work or activities that require concentration can be re-introduced after 24 – 48 hours as long as they do not cause symptoms to come back
- STEP 3: After a further 24 – 48hours if symptoms are not worse, part time return to school can be considered
- STEP 4: After further 24 – 48hours the time spent at school can be increased back to normal full days, provided symptoms do not come back
If symptoms are worsened by new activities, it is important go back a step and lower the intensity of activity for a period of 24 hours.
Symptoms of concussion can come and go and can last for a number of weeks after the injury. If they are present most days for more than a month, seek advice from your doctor.
Contact sports should be avoided until symptoms have resolved completely (and for at least 3 weeks after the injury).
Contact your doctor if:
If:
- You are worried about your child
- Symptoms have changed since being reviewed in the Emergency Department and you are concerned
- Symptoms of headache, change in character or behaviour, difficulty concentrating are longer than 1 week after the head injury
Call 999
If:
- Your child cannot be woken up to normal alertness
- Symptoms have changed since attending the Emergency Department and your child is very unwell
Should you require further advice on the issues contained in this leaflet, please call NHS 111
Staged return to school
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats your child, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to your child. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your child’s condition, the alternatives available for your child, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about your child
We collect and use your child’s information to provide your child with care and treatment. As part of your child’s care, information about your child will be shared between members of a healthcare team, some of whom you may not meet. Your child’s information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide your child with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your child’s doctor, or the person caring for your child.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about your child. For further information visit the following page: Confidential Information about You.
If you need information about your child’s (or a child you care for) health and wellbeing and their care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

