- Reference Number: HEY-303/2020
- Departments: Oncology (Cancer Services), Radiotherapy
- Last Updated: 31 May 2020
Introduction
This leaflet has been produced to give you general information about radiotherapy treatment and is additional to the information you will receive from your clinical oncologist and the healthcare team. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it, you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
You would have been offered the option of radiotherapy alone, or in conjunction with chemotherapy, if you have been diagnosed with cancer of the oesophagus or at the junction of oesophagus and stomach (gastro-oesophageal junction (GOJ)) (see diagram)
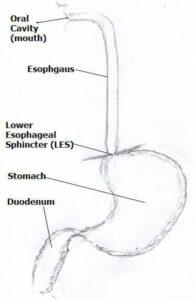
Diagram Courtesy of Dr. R Roy, Consultant Clinical Oncologist
Radiotherapy is the use of high energy X-rays and other types of radiation to treat cancer. Radiotherapy works by causing chemical and physical damage to the cancer cells in the treatment area. Although some normal healthy cells are also affected these are able to recover and repair themselves; unlike the cancer cells which are damaged beyond repair.
Radiotherapy has a number of different benefits. For example, it can be used in combination with chemotherapy as a primary (first) treatment option for oesophageal (gullet) cancer to achieve a cure or long term control; as an additional treatment prior to surgery to improve the cure rate in selected patients, as well as being used in the palliative setting for symptom control, like improving your swallow or reduce the risk of bleeding. Radiotherapy does not make you radioactive and you are safe to be around people including children whilst you are on treatment.
Your oncologist will have discussed the treatment and side effects with you and gained your written consent to receive radiotherapy. There are several stages prior to you actually starting your treatment.
Planning your Radiotherapy Treatment
Your first appointment in the Radiotherapy department is called a planning appointment. This appointment will be approximately 15 – 30 minutes in duration. Further information regarding the planning of your treatment is available in the leaflet ‘Introduction to Radiotherapy CT Planning’.
You may be asked to fast for 2 hours prior to your Computed Tomography (CT) Planning Scan and to drink a cup of water half an hour before the scan. You will then have to repeat this every time you attend for radiotherapy treatment.
Your course of radiotherapy will be, planned on an individual basis using a special CT planning scan. For this scan, you will be laid on a piece of equipment known as an ‘immobilisation board’ (Fig 1). You will be required to lay flat on your back with your arms raised above your head (Fig 2).
The scan may be in the form of single scan or multiple scans taken during different parts of breathing cycle; which will be explained in detail prior to the procedure. It is important that you are comfortable as this will be the position you will be in for your daily treatment. If you are not comfortable, please inform a member of staff at the time so adjustments may be made for your comfort.
For your CT planning and treatment appointments, your upper body will need to be exposed from the waist up. You will be provided with upper body treatment gowns for your convenience but the garment will also have to be opened for treatment.
A member of the support team will discuss skin care and side effect management with you at this appointment. You will also have the opportunity to discuss any concerns or issues you may be having regarding your treatment.
|
|
|
| Fig 1: Showing an immobilisation board | Fig 2: Showing your position on the board |
Permanent Skin Marks
During the initial planning appointment pen marks will be drawn onto your skin, to ‘mark on’ the treatment site. As these pen marks will wash off, we prefer to make very small permanent skin marks before you leave the department. These permanent marks are made using a very fine needle and tattooing ink, and provide a permanent mark that we can use for reference when delivering your radiotherapy treatment. These permanent marks mean you are able to bathe and shower during treatment as normal.
If you had to fast before your CT planning scan you will have to repeat this for all of your radiotherapy treatment appointments.
Every day you attend your radiotherapy treatment please book in at the Radiotherapy reception desk. You will be either asked to take a seat in the main reception waiting area or directed to a specific waiting area.
On your first day of treatment you will be collected from the main waiting area and shown where to sit for future appointments.
Radiotherapy is delivered using a machine called a Linear Accelerator (Fig 3) or Linac for short. Radiotherapy treatment is painless and appointments are usually 10 – 15 minutes long.

| Fig 3: A Linear Accelerator, also known as a ‘Linac’, used to deliver your radiotherapy |
A member of staff will escort you into the treatment room. The treatment machines and rooms are very large and can appear quite overwhelming when you see them for the first time. You will need to undress to the waist (as for your planning scan) unless you are wearing an upper body treatment gown. There is a curtained changing area within the treatment room should you wish to use it and there are changing cubicles adjacent to each machine.
The radiographers will then assist you into the correct treatment position on the couch. This is the same position that you were placed on the immobilisation board during your planning appointment. It will be necessary to open your upper body treatment gown at this point, if you are wearing one, to allow the radiographers to see your ‘permanent skin marks’. The radiographers will move you closer to the machine and will start to move you back into the exact position you were in for your planning scan, using the permanent marks. You will not go inside the machine; it will move around you. The radiographers are controlling the Linac at all times and it will not touch you.
Once you are set up in the correct position, the staff will then leave the room for a few minutes to start delivering the treatment.
The machine will rotate around you in different directions but is being controlled by the staff outside in the control area. The radiographers are watching you at all times on the TV monitors, should you need to attract their attention or if any assistance is required. You will not feel or see anything during your treatment however; you may hear a buzzing sound when the treatment is being delivered.
Typical course of Chemo Radiotherapy or Radical Radiotherapy as a single modality treatment
Your oncologist would have already discussed with you the number of sessions of radiotherapy that you will require in combination with your chemotherapy treatment or as a standalone radiotherapy treatment alone. This is typically between 16 to 25 sessions if the intention of the treatment is to give you a radical course of therapy to facilitate longer-term control. If, however, the purpose of radiotherapy is to improve your cancer related symptoms, you will typically receive between 1 and 10 sessions of radiotherapy. This is not in conjunction with any chemotherapy treatment.
Review appointments during treatment
You will have regular weekly reviews with a radiographer as you progress through your treatment. This is to assess your general health and how you are coping with any side effects, so please be honest in your answers, as this will be documented as an assessment of your treatment. You may be referred to one of our support team if further medical advice or intervention is required. Please do not feel this is the only time you can voice any concerns regarding your health, the radiographers will ask how you are feeling every day before treatment.
Chemotherapy component of the treatment
Radiotherapy for gullet cancer is often given in conjunction with chemotherapy to have the best results. This would have been discussed with you by your oncologist and a detailed plan of treatment including the drugs to be used will have been explained.
If you are not having chemotherapy with your radiotherapy, then this would have also been discussed by your oncologist and explained to you.
Commonly used chemotherapy combinations are:
- Cisplatin and Capecitabine: This is typically given on a 3 weekly schedule where you will receive the drug Cisplatin on Day 1 of your Radiotherapy treatment as an intravenous drip in the chemotherapy day unit and you will be given a supply of Capecitabine tablets for you to take twice a day every day for the entire duration of your radiotherapy. The cisplatin drip will be repeated in 3 weeks’ time. Sometimes, you will receive some chemotherapy on its own for a period of 3 – 6 weeks prior to starting your combination chemotherapy and radiotherapy and this would again have been discussed with you by your oncologist.
- Carboplatin and Paclitaxel: These drugs are given as an intravenous drip on a weekly basis during your radiotherapy treatment and will be delivered in the chemotherapy day treatment unit. During a typical course of chemo-radiation treatment, you will receive between 4 – 5 doses of this chemo over a 4 – 5-week period and your particular situation will be discussed by your oncologist prior to you starting treatment.
- Cisplatin or Carboplatin: Based on your physical fitness and functions of your essential organs like kidneys and liver, your oncologist may recommend just a single drug to be given as an intravenous drip on a weekly basis along with your radiotherapy and like all other chemotherapy drips will be delivered in the chemotherapy day treatment unit. Such decision is taken to minimize the impact of the treatment on you and yet keep the treatment effective for controlling the tumour.
Side effects of treatment
Side effects and reactions from the treatment may be experienced as you progress through your treatment. As every individual is different, you may experience some of these and at varying levels; this is normal and in most cases temporary so please do not worry. You can speak to your radiotherapy or chemotherapy team about your symptoms and we can advise you on how to control them or if they worsen how we can treat you.
Listed below are some of the most common side effects experienced. These usually begin midway into your treatment and may last for several weeks and continue for a short while once you have completed your radiotherapy but will then slowly settle down.
Heartburn and difficulty in swallowing
Patients having this area treated may find some discomfort in swallowing and may feel as if they have a lump in their throat. If this happens, your consultant can prescribe medication to help. For the duration of your treatment, you may find eating softer foods helpful; dietician advice is also available if required. At the later stages of your treatment, you may find it difficult to swallow even soft-food and if you in conjunction with the dietitian are concerned about your nutrition, supplements to be taken orally will be prescribed.
In a smaller number of patients, we may recommend addition feeding via a naso-gastric tube or a RIG tube (a feeding tube placed directly in your stomach under X-ray guidance). If such need arises, it will be fully explained to you before we undertake any such procedures.
Nausea and sickness
You will be given drugs to counteract the nausea and vomiting caused by this treatment. Patients are recommended to drink extra fluid and eat little and often. If these symptoms persist, please inform your treatment radiographers, support team, chemotherapy team who can offer advice or arrange for additional medication to be prescribed.
Skin Reactions
Sometimes radiotherapy may cause skin in the treated area to become pink, itchy or possibly sore. Advice will be given on how to care for your skin if this does happen and the support team may supply a topical cream.
Fatigue
As the treatment progresses, you may feel increasingly tired, especially if you are travelling some distance to the department. It is therefore important to have sufficient rest. Maintaining gentle exercise can also be beneficial. As with all radiotherapy side effects, this varies from person to person. You may feel that you need to sleep or rest with your feet up for a while during the day. It is also important to increase your fluid intake so try and drink every hour. It is not, recommended you to drink alcohol during your treatment, as it will increase the likelihood of dehydration and can often cause additional burning sensation in your gullet.
If you are receiving a short-course of radiotherapy (typically between 1 – 10 sessions / fractions) to palliate the symptoms of cancer, you are less likely to experience significant side-effects. Most commonly observed and experience side-effects are a degree of fatigue lasting 2 weeks, intermittent nausea and occasional vomiting, soreness of the gullet causing a temporary difficulty in swallowing certain food which typically resolves in 2 – 4 weeks. There are no significant longer-term side-effects with a short course of palliative radiotherapy.
Other side effects from your chemotherapy treatment
Common side-effects that are often encountered with the chemotherapy part of your treatment are as follows:
- Hair loss
- Diarrhoea / constipation
- Tummy cramps / pain
- Change in taste sensation
- Mouth soreness and ulcerations involving tongue / lips / gums
- Redness and soreness of hands and feet
- Gritty and watering eyes
- Pins and Needles affecting hands and feet
- Reduced immunity which will make you more susceptible to infection
Around 5 in 100 (5%) of patients may develop central chest discomfort with associated sweating and breathlessness while on certain chemotherapy and if you are experiencing such symptoms, you should be contacting the department at the given numbers without any delay.
A small minority of patients, less than 1 in 100 (1%), may develop significant diarrhoea and mouth ulcers along with sore skin of palms and soles with some blistering and peeling of the skins. It is best to report any problems at its earliest stage for us to be able to monitor closely and offer you the appropriate remedy.
Although every effort is made to identify side-effects at the earliest stages and deal with them satisfactorily, these are potentially toxic treatments and poses significant risk to a person’s health in a small minority of individuals. Before you start your treatment, chemotherapy specialist nurses will be going through these potential side-effects with you in detail and will also provide you with necessary help-line numbers for both in-hours and out-of-hours for you to contact us if you are concerned about any side-effects.
Late effects of radiotherapy can occur once you have completed your course of treatment.
Your consultant will have explained these late effects with you:
- Radiotherapy to this area can cause scarring of the oesophagus and for it to become less elastic. In rare cases, further treatment may be required to improve your swallowing.
- In a small number of patients, less than 1 in 100 (1%), the oesophagus can weaken and the walls become thin. This can result in a small tear occurring that is also a rare late side effect.
- The possibility of developing a dry cough secondary to radiation pneumonitis (inflammation of the lung tissue caused by the radiotherapy) tends to appear 4 – 6 weeks after radiotherapy and can be treated by antibiotics and steroids.
- There is a small risk, less than 3 in 100 (3%), of causing some degree of scarring of the lungs and weakening of the muscle action of the heart and they will be monitored in the longer-term as part of your follow-up.
What happens when I finish treatment?
Once you have completed your course of radiotherapy treatment, you will receive a follow-up appointment with your consultant or a member of their team. This appointment will be sent out in the post for you to return to see your consultant oncologist at the hospital where you were first seen. This is usually around 4 – 6 weeks after treatment has finished, allowing any side effects experienced to settle down. Your consultant will then decide if any further test or appointments are necessary.
General advice and Support Services
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination. Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Radiotherapy Information and Support Team
Telephone number: (01482) 461206
Monday – Friday 8.00am – 6.00pm, excluding weekends and Bank Holidays
Or by email: hyp-tr.radiotherapy.information@nhs.net
Radiotherapy Staff
Clinical Oncologist and Consultant Therapeutic Radiographers
This is your consultant who is an expert in radiotherapy and will be managing your treatment. They will take the responsibility for deciding what dose and how many treatments will be best for you; they will oversee the planning of your treatment. You may see them or a member of their team at your initial planning appointment and you can see them during your treatment if you have any problems or queries.
Therapeutic Radiographers
Radiotherapy is delivered by male and female therapeutic radiographers who are specialist healthcare professionals that are trained to plan and deliver radiotherapy treatment and to use the specialist equipment. You will usually see the same team of radiographers and they will assist you with any questions or problems or refer you to a more appropriate person.
Radiotherapy Support Team
The team consists of registered nurses, radiographers and clinical support workers (CSW’s), who are based within the Radiotherapy Department where they actively support and advise patients receiving radiotherapy treatment. They are able to make appropriate referrals and offer advice to patients and their families / carers.
Physicists, planning dosimetrists and machine technicians
Medical physicists are specialist scientists who have a key role in the individual planning of your treatment, along with the planning technicians. They may also have an input into the set-up of your treatment. They work together with the machine technicians to ensure that the machines are reliable and working accurately.
Students
At some point during your treatment you may encounter student radiographers. Everything they do is supervised fully. If you would prefer our students not to be present during the planning and treatment please let a member of staff know when you attend for your initial planning appointment.
Other members of staff
During your treatment course, you may meet our receptionists, dieticians, oncology health staff, patient services staff, porters, volunteer workers. All are working together to provide you with a high quality of healthcare.
Useful contacts
Health Centre
The primary aim of our health centre is to help patients and their families to have the best possible health and quality of life during and after treatment. It is open to all oncology patients and their families in offering an informal atmosphere to those who wish to “drop in” to the centre. Specially trained staff are able to advise on different aspects of coping with cancer. The centre is located in the Queen’s Centre at Castle Hill Hospital. Opening times are Monday – Friday 9.00am – 5.00pm.
Contact details of useful organisations that provide information about cancer including radiotherapy treatments:
Macmillan Cancer Support
MacMillan Cancer Support provides information from specialist nurses on all aspects of cancer, its treatment and on the practical and emotional aspects of living with cancer.
You can drop into the Macmillan Cancer Information Centre at the Queen’s Centre or call them on (01482) 461154 Monday – Friday 9.00am – 5.00pm.
Alternatively, free phone the national help line: 0808 808 0000 Monday – Friday 9.00am – 8.00pm.
Online: http://www.macmillan.org.uk
Write to Macmillan Cancer Support, 89 Albert Embankment, London, SE1 7UQ
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.


