- Reference Number: HEY-1356-2023
- Departments:
- Last Updated: 1 March 2023
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should have been answered by this leaflet. It is not intended to replace the discussion between you and your doctor/hand therapist, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team who has been caring for you.
What is the central slip?
The central slip makes up part of the extensor tendons of the fingers. The extensor tendons connect the muscles to the bone and are responsible for straightening your fingers. The central slip works on straightening the middle joint of your finger. A cut or injury to these tendons is a serious injury and will require regular hand therapy to regain movement after surgery.
Can there be any complications or risks?
Tendons are complex, intricate structures that are vulnerable following repair up to about 12 weeks. In order for them to function properly following your operation, it is important that you exercise your hand regularly and only as advised. Too much, or incorrect exercise may cause the repaired tendon to snap. Too little exercise may result in the tendons becoming stuck down with scar tissue, making them ineffective or the joints to become stiff limiting range of movement .
Splint and elevation
A splint is made to protect your tendon whilst it heals. It is vital that you DO NOT remove the splint until advised to do so by your doctor or hand therapist.
Swelling is a normal reaction to surgery, however, it is important to limit this as much as possible:
- Wear your sling during the day for the first 3-5 days following surgery
- Keep your hand elevated when wearing your splint
- Elevate your hand on pillows at night
- If your hand remains swollen continue the elevation until it settles
Exercise
The hand therapist will demonstrate the exercises which you should continue to do regularly at home.
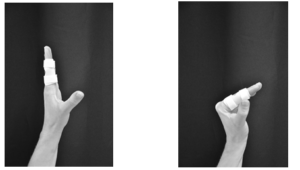
- ACTIVE DIPJOINT FLEXION
Use your unaffected hand to firmly hold the splint between thumb and fingers, bend the tip joint as far as able. Hold 3 seconds before straightening it.

- ACTIVE MCPJOINT FLEXION AND EXTENSION
Bend your fingers from the knuckles, making sure that you keep your fingers straight. Hold for 5 seconds
Repeat the exercise ________ times every ______ hours
General Advice
- You can use your hand for daily activities with the splint remaining in place – however, you should avoid heavy gripping or lifting until advised by your hand therapist.
- Keep your wound and splint clean and dry until advised by your hand therapist – cover in a plastic bag for showering/bathing.
- Don’t do any exercises that the physiotherapist has not shown you.
- Don’t force your finger/s to bend.
- Don’t allow your splint to be exposed to sources of heat as the plastic may melt.
- Don’t try to make alterations to your splint. Contact your hand therapist if you have any issues with the splint.
- It is important you keep the normal movement at all joints that are not splinted – this includes other fingers/thumb, wrist, elbow and shoulder.
Recovery Period
A tendon will repair by forming a scar, rather like a cut on the skin. However, a tendon takes much longer to heal, and remains vulnerable for several weeks after the skin wounds have healed.
This is only a guide and may vary according to individual injuries.
- 0 – 2 weeks Wear the splint at all times – Do exercises in the splint
- 2 – 4 weeks Splint may be removed for gentle exercise of the middle joint up to 45 degrees and then reapplied
- 4 – 6 weeks Splint may be removed for gentle exercise of the middle joint up to 90 degrees and then reapplied
- 6+ weeks Splint may be discarded. Gradually return to normal activities.
- 7+ weeks Return to driving if safe to do so
- 10+ weeks Return to heavy/manual work
- 12+ weeks Return to contact sport
Contact Details
If you have any problems or questions call the Physiotherapy Department on the following telephone numbers:
- Castle Hill Hospital – (01482) 622296 (Monday to Friday)
- Plastic Surgery Trauma Clinic HRI – (01482 674509) – (Daily including weekends and bank holidays)
This leaflet was produced by the Physiotherapy Hand Unit, Hull & East Yorkshire Hospitals NHS Trust and will be reviewed in July 2025
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

